Star Excursion Balance Test
The Star Excursion Balance Test (SEBT) is a dynamic test that requires strength, flexibility, and proprioception. It is a measure of dynamic balance that provides a significant challenge to athletes and physically active individuals.
The test can be used to assess physical performance, but can also be used to screen deficits in dynamic postural control due to musculoskeletal injuries (e.g. chronic ankle instability), to identify athletes at greater risk for lower extremity injury, as well as during the rehabilitation of orthopedic injuries in healthy active adults (1)
Research has suggested to use this test as a screening tool for sport participation as well as a post-rehabilitation test to ensure dynamic functional symmetry.
Figure (physiopedia)

How to perform The SEBT:
Conducting the Test (science for sport)
- The athlete should be wearing lightweight clothing and remove their footwear. After doing so, they are the required to stand in the centre of the star, and await further instruction.
- When using the right foot as the reaching foot, and the left leg to balance, the athlete should complete the circuit in a clockwise fashion. When balancing on the right leg, the athlete should perform the circuit in an anti-clockwise fashion.
- With their hands firmly placed on their hips, the athlete should then be instructed to reach with one foot as far as possible and lightly touch the line before returning back to the starting upright position.
- With a pencil, the test administrator should mark the spot at which the athlete touched the line with their toe. This can then be measured from the centre spot after the test to calculate the reach distance of each reach direction. Reach distances should be recorded to the nearest 0.5cm (22).
- They should then repeat this with the same foot for all reach directions before changing foot.
- After they have completed a full circuit (every reach direction) with each foot, they should then repeat this process for a total of three times per leg. For example, they should have three anterior reach performances for both their right and left leg.
- Once the athlete has performed 3 successful reaches with each foot in all directions, they are then permitted to step away from the testing area.
- The test administrator should have recorded the reach distance of each successful attempt, with a pencil, in order to calculate the athlete’s SEBT score after the test.
Scoring System
With the test complete and all performances measured and recorded, the test administrator can then calculate the athlete’s SEBT performance scores using the following simple equations:
- Average distance in each direction (cm) = Reach 1 + Reach 2 + Reach 3 / 3
- Relative (normalised) distance in each direction (%) = Average distance in each direction / leg length * 100
These calculations should be performed for both the right and left leg in each direction, providing you with a total of 16 scores per athlete.
Normative data
Figure ( Miller, T., 2012).
- According to Hertel, Miller, and Deneger (2000), the reliability of the SEBT ranges between r = 0.85-0.96
- According to Plisky et al (2006), the reliability of this test ranges between 0.82-0.87 and scores 0.99 for the measurement of limb length
- Chaiwanichsiri et al (2005) concluded that the Star Excursion Balance training was more effective than a conventional therapy program in improving functional stability of a sprained ankle
- Plisky et al (2009) concluded that the intra-rater reliability of the SEBT as being moderate to good (ICC 0.67- 0.97) and inter-rater reliability as being poor to good (0.35-0.93) [2]
Supporting Articles/text
Advanced fitness assessment and exercise prescription. Heyward V. Human kinetics, 6th edition: 303 (5)
Miller, T. (2012). National Strength and Conditioning Association. Test and Assessment. Human Kinetics. Champagne, IL.
Bressel E, Yonker JC, Kras J, Heath EM. Comparison of Static and Dynamic Balance in Female Collegiate Soccer, Basketball, and Gymnastics Athletes. Journal of Athletic Training 2007;42(1):42–46.
Chaiwanichsiri D., Lorprayoon E., Noomanoch L. (2005). Star Excursion Balance Training : Effects on Ankle Functional Stability after Ankle Sprain. Journal of Medical Association Thailand 88(4): 90-94 (1B)
Plisky P., Rauh M., Kaminski T., Underwood F (2006) Star Excursion Balance Test as a Predictor of Lower Extremity Injury in High School Basketball Players. Journal of Orthopaedic and Sports Physical Therapy. 36 (12) (1B)
Plisky P et al. (2009). The Reliability of an Instrumented Device for Measuring Components of the Star Excursion Balance Test. American Journal of Sports Physical Therapy. 4(2): 92–99. (2B)

Home > Fitness Testing > Tests > Balance > Star Excursion

Star Excursion Balance Test (SEBT)
The Star Excursion Balance Test (SEBT) is a test of dynamic balance, using in a single-leg stance that requires strength, flexibility, core control and proprioception. The test requires participants to balance on one leg and reach as far as possible in eight different directions. The similar Y-Balance Test was derived from this test.
purpose : To assess active balance and core control
equipment required: A flat, smooth, non-slip surface, measuring tape, marking tape. To prepare for the test, four 120cm lengths of marking tape are placed on to the floor, intersecting in the middle, and with the lines placed at 45-degree angles.
pre-test: Explain the test procedures to the subject. Perform screening of health risks and obtain informed consent. Prepare forms and record basic information such as age, height, body weight, gender, test conditions. Perform an appropriate warm-up. See more details of pre-test procedures .
procedure: The subject should be wearing lightweight and non-restrictive clothing and no footwear. The subject stands on one foot in the center of the star with their hands on their hips. They then reach with one foot as far as possible in one direction and lightly touch the line before returning back to the starting position. The support foot must stay flat on the ground. This is repeated for a full circuit, touching the line in every reach direction. The assessor should mark the spot on the line where the subject was able to reach. The test should be repeated three times for each foot. The trial is invalid if the subject cannot return to the starting position, the foot makes too heavy of a touch, or if the subject loses balance. see video .

Scoring : After the test all the reached distances are recorded to the nearest 0.5cm. Calculate Average distance in each direction (average of the three measurements) and Relative (normalised) distance in each direction (%) (average distance in each direction / leg length * 100). These calculations should be performed for both the right and left leg in each direction, providing a total of 16 scores per athlete.
Comments: this test has been used as an indicator of lower limb injury risk in a variety of populations
advantages: this is a simple test to perform with simple and inexpensive equipment.
disadvantages: the test can be time-consuming if it needs to be performed on a large group of individuals.
The Test in Action
- See a video description of the star excursion balance test
Similar Tests
- A similar test, the y-balance test
Related Pages
- See a video about the Y Balance test
- About balance testing
- Other balance tests
Search This Site
Testing extra.
We have over 400 fitness tests listed, so it's not easy to choose the best one to use. You should consider the validity, reliability, costs and ease of use for each test. Use our testing guide to conducting, recording, and interpreting fitness tests. Any questions, please ask or search for your answer.
Latest Pages
- List of eSports
- Medicine for Weight Loss
- Olympic Flames of the Future
- Sport in Palestine
Current Events
- Tour de France
- Paris Olympics
- 2024 Major Events Calendar
Popular Pages
- Super Bowl Winners
- Ballon d'Or Winners
- World Cup Winners
Latest Sports Added
- Kubihiki - neck pulling
- Wheelchair Cricket
- SUP Jousting
home search sitemap store
SOCIAL MEDIA
newsletter facebook X (twitter )
privacy policy disclaimer copyright
contact author info advertising

- Sign in to save searches and organize your favorite content.
- Not registered? Sign up
Recently viewed (0)
- Save Search
- Next Article
The Star Excursion Balance Test: An Update Review and Practical Guidelines
Click name to view affiliation
- Get Citation Alerts
- Download PDF
The Star Excursion Balance Test (SEBT) is a reliable, responsive, and clinically relevant functional assessment of lower limbs’ dynamic postural control. However, great disparity exists regarding its methodology and the reported outcomes. Large and specific databases from various population (sport, age, and gender) are needed to help clinicians when interpreting SEBT performances in daily practice. Several contributors to SEBT performances in each direction were recently highlighted. The purpose of this clinical commentary is to (a) provide an updated review of the design, implementation, and interpretation of the SEBT and (b) propose guidelines to standardize SEBT procedures for better comparisons across studies.
- ▸ The modified Star Excursion Balance Test (mSEBT) should be used as a reliable clinical tool to assess dynamic postural control. We propose a compact version of the mSEBT for clinicians.
- ▸ All three directions as well as the composite score should be evaluated independently.
- ▸ Procedure consistency is needed (Table 1 ). Scores obtained from Y-Balance Test TM and mSEBT cannot be considered as identical.
- ▸ Key baseline characteristics should be captured among healthy athletes from various sports.
- ▸ It remains unclear whether connections exist between qualitative analysis of mSEBT performance and injury risk.
- ▸ Clinicians should refer to existing Smallest Detectable Changes scores for potentially meaningful cutoffs for injury risk estimates. Important anterior asymmetry should be reported as it might be considered as a potential risk factor for lower-extremity injury.
2021 Updated Recommendations for the SEBT Procedure
Note . ASIS = anterior and superior iliac spine; ANT = anterior; PL = posterolateral; PM = posteromedial; SEBT = Star Excursion Balance Test.
Sport injury prevention is a major goal for sports medicine and performance professionals. 1 Developing meaningful and easily implemented clinical tests to identify at-risk individuals and target them for prevention programs is therefore necessary. 2 The Star Excursion Balance Test (SEBT), initially described by Gray, 3 is a functional test originated from rehabilitation exercises of the lower limb. Since its inception, the SEBT has been frequently described in the scientific literature and evaluated for its ability to (a) assess dynamic postural control of the lower limb, 4 (b) elucidate functional deficits during return to sport phase, 5 – 8 and/or (c) identify at-risk individuals for future injuries. 9 – 11 In their systematic review, Hegedus et al. 12 revealed that across multiple functional assessments, only the SEBT has shown consistent utility for identifying increased injury risk among sport populations. Recently, evidence has emerged to suggest that the SEBT is highly reproducible. 13 The intersession reliability estimates, and smallest detectable changes (SDCs) reported suggest that the SEBT performance is stable over time with a predictable amount of error that can be accounted for in overall performance and in each direction. It is critically important that clinicians have meaningful tools for (a) capturing potential impairments in function that may increase the risk of injury and (b) charting improvements in rehabilitation function. The SEBT appears to have these qualities.
Performance rules of SEBT appear to be heterogeneous among studies. Methodological considerations regarding testing procedures may explain a large part of the observed variability in the SEBT directional values across studies. Indeed, a precise analysis of testing conditions reported in several studies revealed a critical inconsistency due to a lack of standardized procedure. 8 , 10 , 14 , 15 Thus, cutoff scores and smallest detectable differences reported in the literature are blurred, making challenging the interpretation and comparison of scores between samples or studies. 13 , 16 , 17 In 2009, an instrumented device, the Y-Balance Test ™ (YBT), was developed by Plisky et al. 18 in order to help experimenters during data collection. Several research teams have used this tool to evaluate dynamic postural control among various populations. 19 – 22 In their systematic review, Gribble et al. 7 in 2012 provided a starting point for the SEBT and YBT utility in clinical practice. The evidence since this review has substantially evolved. The aim of this commentary is to provide readers with a clinical update from recent evidence concerning SEBT procedure and interpretation with implications for clinical practice. In this commentary, we propose practical recommendations concerning the standardization of the test in order to reduce the variability of the outcomes across studies.
A careful and precise analysis of the procedures revealed important variations in (a) the methodology, (b) the data collection and analysis, and (c) the interpretation of the results. The suggested recommendations will be discussed in the next section. The practical recommendations for the SEBT standardization in order to obtain reliable and comparable results from one study to the other are reported in Table 1 .
- An Overview of Procedures
The SEBT was initially described with the individual standing in the center of eight lines forming an eight-pointed star with 45° between each of them. 23 Several studies revealed that this procedure could be simplified with only three lines (or directions, named according to the stance foot): anterior (ANT), posteromedial (PM), and posterolateral (PL). 7 , 16 , 24 This “simplified” version is now frequently but not systematically, used and named in the literature as the mSEBT. 13 , 25 The mSEBT saves time during testing by avoiding redundancy of testing directions while maintaining consistency and reliability from the original SEBT. 16 , 26 The average of the three directions is then often calculated to create a composite score (COMP). Most clinicians and researchers regularly refer to YBT when describing the test despite there being a trademarked name of a device developed by Plisky et al. 18 (see the specific section below). When carefully analyzing the literature, studies could either refer to SEBT, 10 mSEBT, 5 YBT, 27 or even the Y-Balance Test-Lower Quarter (YBT-LQ) 28 in the title or abstract although the testing procedure was similar.
Although ANT, PM, or PL refer to stance foot (Figure 1 ), some discrepancies exist in the literature when the procedure is carefully examined especially on the PL and PM directions. Indeed, recent publications switched the posterior directions in their descriptions of the procedure. 9 , 19 , 20 , 29 Those mistakes lead to potential misinterpretations of the results (see the cutoff section below). This underlines the importance and necessity for operationally defining the directions and ensuring consistency in the procedure and rigor when reading the studies.

—Setup of the mSEBT grid with three lines SEBT for left and right foot. ANT = anterior; PL = posterolateral; PM = posteromedial; mSEBT = modified Star Excursion Balance Test; SEBT = Star Excursion Balance Test.
Citation: International Journal of Athletic Therapy and Training 26, 6; 10.1123/ijatt.2020-0106
- Download Figure
- Download figure as PowerPoint slide
For the testing procedure, individuals stand barefoot in double limb stance (i.e., feet together) at the center of the testing grid. Participants attempt to reach the maximal distance along each direction with the most distal portion of the reaching foot, touch the directional line, and return while keeping balance on the support. 7 When the participant regains double limb stance after the reach, the trial is over. As hand placement during the test as well as criteria for success remain different across studies, particular instructions and the exact definition of a failed trial will be discussed in specific sections. The obtained distance (typically measured in centimeters) reflects the dynamic postural performance of the stance limb.
- Number of Practice Trials
We recommend that participants should be familiar with the test to prevent any learning effect with this procedure. Several authors studied the number of trials needed to obtain a stable and reliable performance by limiting a learning effect and/or muscular fatigue. The original test was described with six practice trials in every direction for each limb. More recently, this number was lowered to four for each limb in every direction. This number (four) provides reproducible scores without additional warm-up and decreases the procedure duration because maximum performance is normally reached and the lower limb kinematics are usually stabilized. 7 , 15 , 30 , 31
- Number of Recorded Trials
Regarding the assessed parameters, the mean (in centimeters) is calculated from three trials for each direction. Some authors 10 only selected the best performance of the three trials. As reliability of both methods appears to be acceptable, no strict recommendation can be made for this criterion (mean or maximum of the three trials). It appears also relevant to switch the tested limb for each direction to reduce the onset of fatigue. 18 However, it may be worth carefully observing the evolution of performance across trials and potentially asking individuals to repeat attempts until a relative stabilization of scores during three consecutive trials. We therefore recommend that deviation between trials for the same direction on the same foot should not exceed 2 cm (based on the SE of measurement from Powden et al. 17 ).
- Participant Hand and Foot Placement During the SEBT
Another source of inconsistency was linked to both foot and hand placements of participants during SEBT testing. 14 Several investigators described testing procedures with participants maintaining hands on hips throughout the mSEBT reach, 7 , 10 , 32 – 36 while others did not control for hand placement. 6 , 16 , 22 , 23 , 34 The use of upper limbs makes balance control easier during the test, 14 , 37 and so if hands are not maintained on the hips, the participant may compensate or conceal a postural control deficit of the lower limb. 21 Moreover, dynamic postural control varies according to specific sports. Differences in SEBT performance across sports could therefore be linked to some participants using their hands during the test compared with others who did not. This would then create a spurious relationship between sport participation and SEBT performance. Thus, in order to compare several populations (or sports activities), we recommend that participants place their hands on their hips in order to standardize trunk displacement and the consistency of errors when performing the protocol 7 , 14 , 21 (Figure 2 ).

—Position of the subject for the evaluation of the right limb in the posteromedial direction.
With regard to stance foot placement, some variations were reported across studies. In the eight lines version of the SEBT, the foot (i.e., the virtual line between both malleoli) was placed at the center of the grid. 38 Several authors continue to use this alignment for the mSEBT. However, the foot can move due to loss of balance or unexpected fall during failed trials. Small changes during positioning with the ANT reach can make significant differences, therefore the foot-centered position is not recommended as it can lead to misleading results. 14 In order to improve the procedure reliability, two easily reproducible positions are proposed. The first is to position the most distal aspect of the great toe at center of the grid during the entire procedure. 10 , 23 In this case, the foot is in a more posterior position when performing the ANT reach, leading to relatively lower performances in the ANT, but higher on both PM and PL directions compared with the initial foot placement. 14 The second option consists of positioning the foot according the reached direction. 39 For the ANT, the most distal aspect of the great toe is placed at 0; but, for PM and PL directions, the most posterior aspect of the heel is placed at 0. This placement seems to minimize the influence of foot length on performance 7 but leads to significant lower PM, PL, and COMP scores 14 and requires moving the foot during the test, leading to potential errors. Similarly, reported SDCs may be different according to the position of the foot. In order to allow comparisons across studies using different foot placements, building a correction factor could be relevant, based on the foot length. For example, important results from large prospective cohort studies have used the procedure with the toe at 0, 10 , 35 , 36 revealing high PM, PL, and COMP scores. We encourage researchers to determine an accurate proportionality coefficient to account for foot placement between each procedure. Therefore, a consistent foot position should be necessarily used when evaluating various athletes and during longitudinal comparison regardless of the chosen procedure.
- A Proposed Compact Solution
For clinicians who do not have enough space for the entire Y of the mSEBT, we propose a “compact” version of the mSEBT using only a single measurement line to allow space efficiency (Figure 3a and 3b ). However, when using this procedure, the participant is required to change foot position for each direction leading to possible errors. We therefore recommend that the investigator carefully check the foot position before collecting the data. Further reliability studies are needed for this version, but it stands to reason that participants may achieve similar performance values.

—A proposed “compact” version of the mSEBT. (a) With foot position in “toe fixed” at 0 for the three directions and (b) the changing toe/heel position according to the reached direction. mSEBT = modified Star Excursion Balance Test.
- The YBT™ Device
In 2009, Plisky et al. 18 developed an instrumented device showing good to excellent intrarater and interrater reliability (intraclass correlation coefficient [ICC] = .97–1 and .85–.89, respectively). A recent study among adolescent female athletes reported that SDCs for normalized reach distance were 2.4% for the composite score, 2.4% for ANT, 3.2% for PM, and 3.2% for PL directions. 40 However, it seems that results obtained with the YBT ™ are not systematically comparable with those obtained with the standard SEBT. 25 , 28 , 32 Fullam et al. 31 recently detailed that main differences related to ANT direction with the YBT ™ leading to significant lower values compared with ANT direction of the SEBT. Similarly, Ko et al. 41 reported significant differences between mSEBT and YBT in individuals with chronic ankle instability in ANT and PM directions. In order to compare scores across studies, it is important to assess if the YBT or the mSEBT was utilized, as outcomes from these two procedures are not interchangeable.
Interpretation of Data
- Criteria for Success
Several general considerations should be applied to validate the trial. Participants have typically been asked to lightly touch the directional line while maintaining both hands on the hips (see related section). They have not been allowed to shift weight on the reaching limb, 15 , 42 lose their balance, or fall. Plisky et al. 18 allowed the stance foot to move or lift during the YBT so that the rater does not need to control it, thereby simplifying the evaluation of the test. However, it is recommended to forbid moving or lifting the heel of the stance foot 7 during the mSEBT in order to increase validity of the procedure. Specifically, during the ANT reach, participants might lift their heel to compensate for impaired weight-bearing ankle dorsiflexion. 17 , 18 There is mounting evidence that ankle dorsiflexion accounts for a significant proportion of ANT direction. 42 , 43 As a decreased range of motion in that direction is considered an important risk factor for ankle sprains, 44 we recommend not lifting the stance foot during the procedure.
- Reliability
Several investigators have reported excellent intra and interrater reliability regarding all three directions (ICC intra = .85–.91 and ICC inter = .99–1). 18 , 23 , 26 , 32 , 38 , 45 – 47 A recent systematic review also revealed that in healthy adults, both mSEBT and YBT have excellent intra and interrater reliability for each direction. 17 Median ICC values for interrater reliability were .88 (from .83 to .96), .87 (from .80 to 1.00), and .88 (from .73 to 1.00) for the ANT, PM, and PL directions, respectively. Concerning intrarater reliability, median ICC values were .88 (from .84 to .93), .88 (from = .85 to .94), and .90 (from .68 to .94) for the ANT, PM, and PL directions, respectively. 17 These ICC values suggest that performance measures are relatively consistent between sessions and raters. In addition, excellent reliability estimates have been reported for both mSEBT (ICC from .87 to .93) 13 and YBT (ICC from .85 to .93) 47 when comparing raters with various qualifications.
- Responsiveness: The SDC
Regarding the SDCs (the smallest amount of change, which falls outside the measurement error of the instrument) in clinical practice, a meaningful change of normalized reach distance (see below for normalization recommendations) should exceed 5.9%, 7.8%, and 7.6% for ANT, PM, and PL directions respectively 17 (Table 2 ). When using nonnormalized reach distances, a minimum of 6.4, 7.1, and 8.8 cm for ANT, PM, and PL directions is necessary to consider a clinically relevant change in healthy adults. 17 It is also suggested that there can be differences in SDC between limbs. 13 When focusing only on the COMP, van Lieshout et al. 13 calculated intrarater SDCs of 7.2% and 6.2% and interrater SDCs of 6.9% and 5% for both right and left leg, respectively, from recreational athletes between 18 and 30 years old.
SDC for Normalized Reach Distances
Note . SDC = smallest detectable changes; SEBT = Star Excursion Balance Test; YBT = Y-Balance Test ™ .
a Averaged SDCs in case of different limb values.
- Normalization With Respect to the Lower Limb

—Preferred measurement of lower limb length. From ASIS to the medial malleolus. Lateral malleolus measurement provides trivial differences. 21 ASIS = anterior and superior iliac spine.
- Composite Score Calculation
This value (in percentage) reflects the overall dynamic postural performance of the tested lower limb. 7 , 10
- Interpretation and relevant comparison
Several intrinsic factors can influence SEBT performances between participants, such as sex, 36 , 50 age, 51 level of play, 52 and injury history 6 , 53 (Table 3 ). Moreover, understanding the Specific Adaptations to Imposed Demands principle, type of sport also influences SEBT values 36 , 54 (Table 3 ). Caution should be taken when comparing outcomes across different populations. Some normative data have been established, 36 , 52 these data sets may however not be large enough to reflect accurate normative values for these different populations. Large databases from healthy participants are therefore needed to allow relevant comparison with what is considered “normal” SEBT performance within each sport. We also insist on the importance of capturing individuals baseline characteristics to identify changes over time from an injury risk or risk reduction standpoint. However, when the athlete baseline status is not available for clinicians, we recommend searching for existing databases among similar healthy individuals. 36 , 52
2021 Updated List of Intrinsic Factors Influencing SEBT Performance Between Individuals
Note . ANT = anterior; PL = posterolateral; PM = posteromedial; SEBT = Star Excursion Balance Test.
- Means and Cutoff Scores
Although it remains unclear what contributes to maintaining the postural control necessary to perform the SEBT, many studies have documented links between mSEBT performance and injury. 10 , 22 , 35
In order to target at-risk athletes for lower limb injuries, cutoff scores are needed. However, while the SDCs have been established, the actual predictive values for reach distances for athletes who are at risk of future injuries are widely different across studies. 10 , 35 Plisky et al. 10 were the first to establish cutoff scores among 235 high school and collegiate basketball players. Females who displayed a normalized composite score below 94% were 6.5 times more at risk of sustaining lower limb injury during the season. For males, the risk was three times higher among players who did not reached 94% of the lower limb length. When focusing on each direction, Attenborough et al., 30 revealed that a PM normalized score below 77.5% is associated with an increased risk of lateral ankle sprain in 94 netball players (odd ratio = 4.04, 95% confidence interval [1.00, 16.35]) while de Noronha et al. 9 showed that higher PL normalized scores above 80% decreased ankle sprain risk among 125 participants (hazard ratio = 0.96, 95% confidence interval [0.92, 0.99]). As previously mentioned, the description of the PL direction in the de Noronha et al. 9 , 30 studies was actually the PM direction described in the Attenborough et al. 30 study. When viewed through this lens, the findings are very similar and highlight the need for careful examination of testing procedure description. In addition, side to side asymmetry appears to be an important characteristic for the injury risk profile. Indeed, an absolute asymmetry ≥4 cm in the ANT direction was associated with a 2.5 times increased risk of lower limb injuries for both males and females. 10 More recently, Stiffler et al. 35 showed that a normalized asymmetry >4.5% in the ANT direction could identify athletes at increased risk of lower-extremity injury with 82% accuracy ( n = 147 healthy National Collegiate Athletic Association athletes). However, side to side asymmetry did not benefit identifying at-risk individuals among 59 football players. 22 Further studies are needed to clarify the relationship between injury risk and mSEBT performances. When evaluating healthy athletes, several research teams 16 , 42 , 50 , 55 did not reveal any differences between dominant and nondominant foot on SEBT performances (Table 3 ). Those results suggest that contrary to what one might think, athletes do not perform better on their dominant limb. Clinicians therefore should check for potentially meaningful performance asymmetry during baseline screening test and return to sports evaluations.
- Contributing Factors Between SEBT Directions
The SEBT reflect the dynamic postural control of the lower limb; however, it remains somewhat unclear what contributes to the performance, whether it be the kinematics of the ankle, knee, or hip strength and coordination of the lower-extremity muscles important for maintaining postural control, or the sensorimotor elements of global postural control. 7 As previously mentioned 31 and recently confirmed by Gabriner et al., 33 weight-bearing ankle dorsiflexion is considered as the main contributor to the ANT performance. Interestingly, PL and PM were conversely influenced by frontal stabilization component, such as evertor strength, medio-lateral postural stability, and proximal function. 27 , 56 We therefore recommend investigating performance in each direction in addition to the composite score. Thus, clinicians should explore arthrokinematics alterations at the ankle for low ANT scores, and neuromuscular deficits in the frontal plane when patients exhibited low PL and PM scores.
- Qualitative Analysis
Finally, most of studies used maximum reach distance as the main quantitative parameter; while, recent findings suggest that maximal performance may not be the only relevant outcome. Indeed, qualitative analysis of the movement (i.e., excursion from sagittal plane, excessive knee valgus, trunk rotation, etc.) may play important roles when assessing individuals. 57 , 58 Further studies are needed to better understand compensations as well as kinetic and kinematic alterations among injured and at-risk athletes for musculoskeletal pathologies, such as patellofemoral or heel pain. 59 , 60 Indeed, kinetic and kinematic alterations are frequent among symptomatic patients and qualitative analysis during the test could help practitioners to identify deficits at baseline, improvements following rehabilitation, and help clinicians regarding return to sport decision. Clinicians could also further use collected qualitative information as useful feedback to improve instructions delivered to the patient during dynamic postural balance exercises. Thus, we encourage clinicians to evaluate the quality of performance of each reach direction 13 , 16 , 17 and if possible, to use one of the numerous available free software programs for further accurate kinematic analysis. Further studies are needed to evaluate the relevance of qualitative analysis for clinicians.
The SEBT is a valid and reliable functional tool to evaluate dynamic postural control of the lower limb. However, transparency in reporting of the SEBT procedures are required to ensure comparable results across studies. Key to this transparency are six recommendations:
- (a) Clinicians should utilize the three reach directions of the mSEBT (ANT, PM, and PL) for the assessment of dynamic postural control. We have proposed a compact version of the mSEBT for clinicians.
- (b) These directions should be evaluated independently as they each provide information about the postural control profile and contributors to postural performance. A composite score should not be the only variable reported.
- (c) Overall instructions need to be standardized especially regarding foot/hand position, number of practice and recorded trials as well as proper identification of posterior directions according to the tested limb. We recommend that clinicians should not use scores from YBT ™ and mSEBT interchangeably.
- (d) Normative values should be captured among heterogenous healthy populations according to sport, gender, and level of play.
- (e) Further studies are needed regarding the qualitative analysis of the test.
- (f) Individual performance should be evaluated using the established SDC scores. Important anterior asymmetry should be carefully reported and might be considered as a potential risk factor for lower-extremity injury.
Large normative databases developed from the consistent use of transparent mSEBT procedures are needed in order to help clinicians to interpret the obtained scores with peers’ samples, and to target at-risk individuals for future injuries, or to better plan the return to sport process. The mSEBT is a clinically meaningful test for assessing dynamic postural control that can be easily implemented. By encouraging clinicians to use the same performance tests with known performance estimates, SDCs, and cutoff scores for risk, it may be possible to develop more robust prevention strategies for sport injuries.
- Acknowledgments
This study did not receive any external funding. The authors have no disclosures or conflict of interest to report.
Vriend I , Gouttebarge V , Finch CF , van Mechelen W , Verhagen EALM . Intervention strategies used in sport injury prevention studies: a systematic review identifying studies applying the Haddon matrix . Sports Med . 2017 ; 47 ( 10 ): 2027 – 2043 . PubMed ID: 28303544 doi:10.1007/s40279-017-0718-y
- Search Google Scholar
- Export Citation
Dallinga JM , Benjaminse A , Lemmink KAPM . Which screening tools can predict injury to the lower extremities in team sports?: a systematic review . Sports Med Auckl NZ . 2012 ; 42 ( 9 ): 791 – 815 . doi:10.2165/11632730-000000000-00000
Gray GW . Lower Extremity Functional Profile . Adrian, MI: Wynn Marketing, Inc ; 1995 .
Gribble PA , Hertel J , Denegar CR , Buckley WE . The effects of fatigue and chronic ankle instability on dynamic postural control . J Athl Train . 2004 ; 39 ( 4 ): 321 – 329 . PubMed ID: 15592604
Clagg S , Paterno MV , Hewett TE , Schmitt LC . Performance on the modified star excursion balance test at the time of return to sport following anterior cruciate ligament reconstruction . J Orthop Sports Phys Ther . 2015 ; 45 ( 6 ): 444 – 452 . PubMed ID: 25899211 doi:10.2519/jospt.2015.5040
Domingues PC , Serenza FS , Muniz TB , et al . The relationship between performance on the modified star excursion balance test and the knee muscle strength before and after anterior cruciate ligament reconstruction . The Knee . 2018 ; 25 ( 4 ): 588 – 594 . PubMed ID: 29886009 doi:10.1016/j.knee.2018.05.010
Gribble PA , Hertel J , Plisky P . Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review . J Athl Train . 2012 ; 47 ( 3 ): 339 – 357 . PubMed ID: 22892416 doi:10.4085/1062-6050-47.3.08
Olmsted LC , Carcia CR , Hertel J , Shultz SJ . Efficacy of the star excursion balance tests in detecting reach deficits in subjects with chronic ankle instability . J Athl Train . 2002 ; 37 ( 4 ): 501 . PubMed ID: 12937574
de Noronha M , França LC , Haupenthal A , Nunes GS . Intrinsic predictive factors for ankle sprain in active university students: a prospective study . Scand J Med Sci Sports . 2013 ; 23 ( 5 ): 541 – 547 . PubMed ID: 22260485 doi:10.1111/j.1600-0838.2011.01434.x
Plisky PJ , Rauh MJ , Kaminski TW , Underwood FB . Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players . J Orthop Sports Phys Ther . 2006 ; 36 ( 12 ): 911 – 919 . PubMed ID: 17193868 doi:10.2519/jospt.2006.2244
Smith CA , Chimera NJ , Warren M . Association of y balance test reach asymmetry and injury in division I athletes . Med Sci Sports Exerc . 2015 ; 47 ( 1 ): 136 – 141 . PubMed ID: 24870573 doi:10.1249/MSS.0000000000000380
Hegedus EJ , McDonough SM , Bleakley C , Baxter D , Cook CE . Clinician-friendly lower extremity physical performance tests in athletes: a systematic review of measurement properties and correlation with injury. Part 2—the tests for the hip, thigh, foot and ankle including the star excursion balance test . Br J Sports Med . 2015 ; 49 ( 10 ): 649 – 656 . PubMed ID: 25614536 doi:10.1136/bjsports-2014-094341
van Lieshout R , Reijneveld EAE , van den Berg SM , et al . Reproducibility of the modified star excursion balance test composite and specific reach direction scores . Int J Sports Phys Ther . 2016 ; 11 ( 3 ): 356 – 365 . PubMed ID: 27274422
Cuğ M . Stance foot alignment and hand positioning alter star excursion balance test scores in those with chronic ankle instability: what are we really assessing? Physiother Theory Pract . 2017 ; 33 ( 4 ): 316 – 322 . PubMed ID: 28362143 doi:10.1080/09593985.2017.1302028
Kaminski TW , Gribble P . The star excursion balance test as a measurement tool . Athl Ther Today . 2003 ; 8 ( 2 ): 46 – 47 . doi:10.1123/att.8.2.46
Hertel J , Braham RA , Hale SA , Olmsted-Kramer LC . Simplifying the star excursion balance test: analyses of subjects with and without chronic ankle instability . J Orthop Sports Phys Ther . 2006 ; 36 ( 3 ): 131 – 137 . PubMed ID: 16596889 doi:10.2519/jospt.2006.36.3.131
Powden CJ , Dodds TK , Gabriel EH . The reliability of the star excursion balance test and lower quarter Y-balance test in healthy adults: a systematic review . Int J Sports Phys Ther . 2019 ; 14 ( 5 ): 683 – 694 . PubMed ID: 31598406 doi:10.26603/ijspt20190683
Plisky PJ , Gorman PP , Butler RJ , Kiesel KB , Underwood FB , Elkins B . The reliability of an instrumented device for measuring components of the star excursion balance test . North Am J Sports Phys Ther NAJSPT . 2009 ; 4 ( 2 ): 92 – 99 .
Ambegaonkar JP , Cortes N , Caswell SV , Ambegaonkar GP , Wyon M . Lower extremity hypermobility, but not core muscle endurance influences balance in female collegiate dancers . Int J Sports Phys Ther . 2016 ; 11 ( 2 ): 220 – 229 . PubMed ID: 27104055
Ambegaonkar JP , Mettinger LM , Caswell SV , Burtt A , Cortes N . Relationships between core endurance, hip strength, and balance in collegiate female athletes . Int J Sports Phys Ther . 2014 ; 9 ( 5 ): 604 – 616 . PubMed ID: 25328823
Hébert-Losier K . Clinical implications of hand position and lower limb length measurement method on Y-balance test scores and interpretations . J Athl Train . 2017 ; 52 ( 10 ): 910 – 917 . PubMed ID: 28937801 doi:10.4085/1062-6050-52.8.02
Butler RJ , Lehr ME , Fink ML , Kiesel KB , Plisky PJ . Dynamic balance performance and noncontact lower extremity injury in college football players: an initial study . Sports Health Multidiscip Approach . 2013 ; 5 ( 5 ): 417 – 422 . doi:10.1177/1941738113498703
Hertel J , Miller SJ , Denegar CR . Intratester and intertester reliability during the star excursion balance tests . J Sport Rehabil . 2000 ; 9 ( 2 ): 104 – 116 . doi:10.1123/jsr.9.2.104
Hertel J . Sensorimotor deficits with ankle sprains and chronic ankle instability . Clin Sports Med . 2008 ; 27 ( 3 ): 353 – 370 . PubMed ID: 18503872 doi:10.1016/j.csm.2008.03.006
Bulow A , Anderson JE , Leiter JR , MacDonald PB , Peeler J . The modified star excursion balance test and Y-balance test results differ when assessing physically active healthy adolescent females . Int J Sports Phys Ther . 2019 ; 14 ( 2 ): 192 – 203 . PubMed ID: 30997272
Robinson RH , Gribble PA . Support for a reduction in the number of trials needed for the star excursion balance test . Arch Phys Med Rehabil . 2008 ; 89 ( 2 ): 364 – 370 . PubMed ID: 18226664 doi:10.1016/j.apmr.2007.08.139
DeJong AF , Mangum LC , Hertel J . Ultrasound imaging of the gluteal muscles during the Y-balance test in individuals with or without chronic ankle instability . J Athl Train . 2020 ; 55 ( 1 ): 49 – 57 . PubMed ID: 31876453 doi:10.4085/1062-6050-363-18
Jagger K , Frazier A , Aron A , Harper B . Scoring performance variations between the Y-Balance test, a modified Y-Balance test, and the modified Star Excursion Balance Test . Int J Sports Phys Ther . 2020 ; 15 ( 1 ): 34 – 41 . PubMed ID: 32089956
Gribble PA , Terada M , Beard MQ , et al . Prediction of lateral ankle sprains in football players based on clinical tests and body mass index. prediction of lateral ankle sprains in football players based on clinical tests and body mass index . Am J Sports Med . 2016 ; 44 ( 2 ): 460 – 467 . PubMed ID: 26646517 doi:10.1177/0363546515614585
Attenborough AS , Sinclair PJ , Sharp T , et al . The identification of risk factors for ankle sprains sustained during netball participation . Phys Ther Sport . 2017 ; 23 : 31 – 36 . PubMed ID: 27665248 doi:10.1016/j.ptsp.2016.06.009
Fullam K , Caulfield B , Coughlan GF , Delahunt E . Kinematic analysis of selected reach directions of the star excursion balance test compared with the Y-balance test . J Sport Rehabil . 2014 ; 23 ( 1 ): 27 – 35 . PubMed ID: 23945793 doi:10.1123/JSR.2012-0114
Coughlan GF , Fullam K , Delahunt E , Gissane C , Caulfield BM . A comparison between performance on selected directions of the star excursion balance test and the Y balance test . J Athl Train . 2012 ; 47 ( 4 ): 366 – 371 . PubMed ID: 22889651 doi:10.4085/1062-6050-47.4.03
Gabriner ML , Houston MN , Kirby JL , Hoch MC . Contributing factors to Star Excursion Balance Test performance in individuals with chronic ankle instability . Gait Posture . 2015 ; 41 ( 4 ): 912 – 916 . PubMed ID: 25845724 doi:10.1016/j.gaitpost.2015.03.013
Munro AG , Herrington LC . Between-session reliability of the star excursion balance test . Phys Ther Sport . 2010 ; 11 ( 4 ): 128 – 132 . PubMed ID: 21055706 doi:10.1016/j.ptsp.2010.07.002
Stiffler MR , Bell DR , Sanfilippo JL , Hetzel SJ , Pickett KA , Heiderscheit BC . Star excursion balance test anterior asymmetry is associated with injury status in division I collegiate athletes . J Orthop Sports Phys Ther . 2017 ; 47 ( 5 ): 339 – 346 . PubMed ID: 28355980 doi:10.2519/jospt.2017.6974
Stiffler MR , Sanfilippo JL , Brooks MA , Heiderscheit BC . Star excursion balance test performance varies by sport in healthy division I collegiate athletes . J Orthop Sports Phys Ther . 2015 ; 45 ( 10 ): 772 – 780 . PubMed ID: 26304643 doi:10.2519/jospt.2015.5777
Marigold DS , Bethune AJ , Patla AE . Role of the unperturbed limb and arms in the reactive recovery response to an unexpected slip during locomotion . J Neurophysiol . 2003 ; 89 ( 4 ): 1727 – 1737 . PubMed ID: 12611998 doi:10.1152/jn.00683.2002
Kinzey SJ , Armstrong CW . The reliability of the star-excursion test in assessing dynamic balance . J Orthop Sports Phys Ther . 1998 ; 27 ( 5 ): 356 – 360 . PubMed ID: 9580895 doi:10.2519/jospt.1998.27.5.356
Earl JE , Hertel J . Lower-extremity muscle activation during the star excursion balance tests . J Sport Rehabil . 2001 ; 10 ( 2 ): 93 – 104 . doi:10.1123/jsr.10.2.93
Greenberg ET , Barle M , Glassmann E , Jung M-K . Interrater and test-retest reliability ofthe Y Balance Test in healthy, early adolescent female athetes . Int J Sports Phys Ther . 2019 ; 14 ( 2 ): 204 – 213 . PubMed ID: 30997273
Ko J , Wikstrom EA , Li Y , Weber M , Brown CN . Performance differences between the modified star excursion balance test and the Y-balance test in individuals with chronic ankle instability . J Sport Rehabil . 2019 ; 29 ( 6 ): 748 – 753 . doi:10.1123/jsr.2018-0078
Gribble PA , Hertel J . Considerations for normalizing measures of the star excursion balance test . Meas Phys Educ Exerc Sci . 2003 ; 7 ( 2 ): 89 – 100 . doi:10.1207/S15327841MPEE0702_3
Hoch MC , Staton GS , McKeon PO . Dorsiflexion range of motion significantly influences dynamic balance . J Sci Med Sport . 2011 ; 14 ( 1 ): 90 – 92 . PubMed ID: 20843744 doi:10.1016/j.jsams.2010.08.001
Vuurberg G , Hoorntje A , Wink LM , et al . Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline . Br J Sports Med . 2018 ; 52 ( 15 ): 956 – 956 . PubMed ID: 29514819 doi:10.1136/bjsports-2017-098106
Hyong IH , Kim JH . Test of intrarater and interrater reliability for the star excursion balance test . J Phys Ther Sci . 2014 ; 26 ( 8 ): 1139 – 1141 . PubMed ID: 25202168 doi:10.1589/jpts.26.1139
Gribble PA , Kelly SE , Refshauge KM , Hiller CE . Interrater reliability of the star excursion balance test . J Athl Train . 2013 ; 48 ( 5 ): 621 – 626 . PubMed ID: 24067151 doi:10.4085/1062-6050-48.3.03
Shaffer SW , Teyhen DS , Lorenson CL , et al . Y-Balance test: a reliability study involving multiple raters . Mil Med . 2013 ; 178 ( 11 ): 1264 – 1270 . PubMed ID: 24183777 doi:10.7205/MILMED-D-13-00222
Neelly K , Wallmann HW , Backus CJ . Validity of measuring leg length with a tape measure compared to a computed tomography scan . Physiother Theory Pract . 2013 ; 29 ( 6 ): 487 – 492 . PubMed ID: 23289961 doi:10.3109/09593985.2012.755589
Filipa A , Byrnes R , Paterno MV , Myer GD , Hewett TE . Neuromuscular training improves performance on the star excursion balance test in young female athletes . J Orthop Sports Phys Ther . 2010 ; 40 ( 9 ): 551 – 558 . PubMed ID: 20710094 doi:10.2519/jospt.2010.3325
Cug M , Wikstrom EA , Golshaei B , Kirazci S . The effects of sex, limb dominance, and soccer participation on knee proprioception and dynamic postural control . J Sport Rehabil . 2016 ; 25 ( 1 ): 31 – 39 . PubMed ID: 26355541 doi:10-1123/jsr.2014-0250
McCann RS , Kosik KB , Beard MQ , Terada M , Pietrosimone BG , Gribble PA . Variations in star excursion balance test performance between high school and collegiate football players . J Strength Cond Res . 2015 ; 29 ( 10 ): 2765 – 2770 . PubMed ID: 25785704 doi:10.1519/JSC.0000000000000947
Vitale JA , Vitale ND , Cavaleri L , et al . Level- and sport-specific Star Excursion Balance Test performance in female volleyball players . J Sports Med Phys Fitness . 2019 ; 59 ( 5 ): 733 – 742 . PubMed ID: 30317834 doi:10.23736/S0022-4707.18.08691-7
Doherty C , Bleakley C , Hertel J , Caulfield B , Ryan J , Delahunt E . Dynamic balance deficits in individuals with chronic ankle instability compared to ankle sprain copers 1 year after a first-time lateral ankle sprain injury . Knee Surg Sports Traumatol Arthrosc . 2016 ; 24 ( 4 ): 1086 – 1095 . PubMed ID: 26254090 doi:10.1007/s00167-015-3744-z
Bressel E , Yonker JC , Kras J , Heath EM . Comparison of static and dynamic balance in female collegiate soccer, basketball, and gymnastics athletes . J Athl Train . 2007 ; 42 ( 1 ): 42 – 46 . PubMed ID: 17597942
Thorpe JL , Ebersole KT . Unilateral balance performance in female collegiate soccer athletes . J Strength Cond Res . 2008 ; 22 ( 5 ): 1429 – 1433 . PubMed ID: 18714247 doi:10.1519/JSC.0b013e31818202db
McCann RS , Crossett ID , Terada M , Kosik KB , Bolding BA , Gribble PA . Hip strength and star excursion balance test deficits of patients with chronic ankle instability . J Sci Med Sport . 2017 ; 20 ( 11 ): 992 – 996 . PubMed ID: 28595864 doi:10.1016/j.jsams.2017.05.005
Pionnier R , Découfour N , Barbier F , Popineau C , Simoneau-Buessinger E . A new approach of the Star Excursion Balance Test to assess dynamic postural control in people complaining from chronic ankle instability . Gait Posture . 2016 ; 45 : 97 – 102 . PubMed ID: 26979889 doi:10.1016/j.gaitpost.2016.01.013
de la Motte S , Arnold BL , Ross SE . Trunk-rotation differences at maximal reach of the star excursion balance test in participants with chronic ankle instability . J Athl Train . 2015 ; 50 ( 4 ): 358 – 365 . PubMed ID: 25531142 doi:10.4085/1062-6050-49.3.74
Willy RW , Hoglund LT , Barton CJ , et al . Patellofemoral pain . J Orthop Sports Phys Ther . 2019 ; 49 ( 9 ): CPG1 – CPG95 . doi:10.2519/jospt.2019.0302
Martin RL , Davenport TE , Reischl SF , et al . Heel pain—plantar fasciitis: Revision 2014 . J Orthop Sports Phys Ther . 2014 ; 44 ( 11 ): A1 – A33 . doi:10.2519/jospt.2014.0303
* Picot is with the French Handball Federation, Créteil, France. Picot, Terrier, and Fourchet are with the French Society of Sport Physiotherapist (SFMKS Lab), Pierrefitte sur Seine, France. Picot, Terrier, and Forestier are with the Savoie Mont-Blanc University, Chambéry, France. Picot, Forestier, and Fourchet are also with the Laboratoire Interuniversitaire de la Biologie et de la Motricité (LIBM), Chambéry, France. Terrier is also with the Whergo SARL, Technolac, France. Fourchet is also with the Hôpital de La Tour, Geneva, Switzerland. McKeon is with the Department of Exercise Science and Athletic Training, Ithaca College, Ithaca, NY, USA.
International Journal of Athletic Therapy and Training
Related Articles
Article sections.
- View raw image
- Download Powerpoint Slide
Article Metrics
- Brice Picot
- Romain Terrier
- Nicolas Forestier
- François Fourchet
- Patrick O. McKeon
Google Scholar
© 2024 Human Kinetics
Powered by:
- [66.249.64.20|185.66.14.133]
- 185.66.14.133
Character limit 500 /500

Star Excursion Balance Test
The Star Excursion Balance Test (SEBT) is a simple, but time intensive, test used to measure dynamic balance/dynamic postural control.
By Owen Walker Last updated: February 29th, 2024 8 min read
Contents of Article
What is the Star Excursion Balance Test?
Why is balance important in sports, how do you conduct the star excursion balance test, what is the star excursion balance test scoring system, is the star excursion balance test valid and reliable, further reading.
- About the Author
The Star Excursion Balance Test was developed to be a reliable measure of dynamic stability. Since then, it has proven to be a sensitive indicator of lower limb injury risk in a variety of populations. To add to this, the Star Excursion Balance Test has been shown to have high levels of intra-rater test-retest reliability , though no validity coefficients have been studied.
The Star Excursion Balance Test (SEBT) is a relatively simple, but somewhat time-intensive, test used to measure dynamic balance, otherwise known as dynamic postural control (1). It measures dynamic balance by challenging athletes to balance on one leg and reach as far as possible in eight different directions (2). Though the SEBT is very similar to the Y Balance Test TM , it is important to understand that these are in fact different, with the Y Balance Test TM being a newer and condensed version of the SEBT.
Performance on the SEBT has been shown to differentiate between individuals with lower limb conditions such as chronic ankle instability (3-10), patellofemoral pain (11), and anterior cruciate ligament reconstruction (12). To add to this, the SEBT is even capable of assessing improvements in dynamic balance following training interventions (13, 14).
Perhaps the SEBT’s greatest talent is its ability to identify athletes with a higher risk of lower limb injury. For example, an anterior reach asymmetry of greater than 4cm during the SEBT has been suggested to predict which individuals are at higher risk of lower limb injury (15). However, other researchers have found that only female athletes with a composite score of less than 94 % of limb length were at greater risk of injury (15). More recent research in collegiate American football players has shown that athletes with a composite score of less than 90 % are 3.5 times more likely to sustain an injury (16).
All of this information suggests that each sport and population (e.g. gender) appear to have their own injury risk cut-off point (15, 16).
Balance, otherwise known as ‘postural control’, can be defined statically as the ability to maintain a base of support with minimal movement, and dynamically as the ability to perform a task while maintaining a stable position (17, 18). In a chaotic sporting environment, the ability to maintain a stable position is vital not only for successful application of the skill but to also reduce the likelihood of injury (15, 16, 19).
As dynamic balance is an integral part of performance, and poor balance is related to a higher risk of injury (20, 21, 15), then it may be of great interest to test and monitor an athlete’s dynamic stability.
It is important to understand that whenever fitness testing is performed, it must be done so in a consistent environment (e.g. facility) so it is protected from varying weather types, and with a dependable surface that is not affected by wet or slippery conditions. If the environment is not consistent, the reliability of repeated tests at later dates can be substantially hindered and result in worthless data.
Required Equipment Before the start of the test, it is important to ensure you have the following items:
- Reliable and consistent testing facility (minimum 2×2 metres (m)).
- Test administrator(s)
- Sticky tape (minimum 8m)
- Measuring tape
- Performance recording sheet
Test Configuration Video 1 displays the test configuration for the SEBT. This setup must be adhered to if accurate and reliable data is desired. The test administrator should stick four 120 cm lengths of sticky tape onto the floor, intersecting in the middle, and with the lines placed at 45° angles (2).
Participants should thoroughly warm up prior to the commencement of the test. Warm-ups should correspond to the biomechanical and physiological nature of the test. In addition, sufficient recovery (e.g. 3-5 minutes) should be administered following the warm-up and prior to the commencement of the test.
Conducting the test
- The athlete should be wearing lightweight clothing and remove their footwear. After doing so, they are then required to stand in the centre of the star and await further instruction.
- When using the right foot as the reaching foot, and the left leg to balance, the athlete should complete the circuit in a clockwise fashion. When balancing on the right leg, the athlete should perform the circuit in an anti-clockwise fashion.
- With their hands firmly placed on their hips, the athlete should then be instructed to reach with one foot as far as possible and lightly touch the line before returning back to the starting upright position.
- With a pencil, the test administrator should mark the spot at which the athlete touched the line with their toe. This can then be measured from the centre spot after the test to calculate the reach distance of each reach direction. Reach distances should be recorded to the nearest 0.5cm (22).
- They should then repeat this with the same foot for all reach directions before changing foot.
- After they have completed a full circuit (every reach direction) with each foot, they should then repeat this process for a total of three times per leg. For example, they should have three anterior reach performances for both their right and left leg.
- Once the athlete has performed three successful reaches with each foot in all directions, they are then permitted to step away from the testing area.
- The test administrator should have recorded the reach distance of each successful attempt, with a pencil, in order to calculate the athlete’s SEBT score after the test.
NOTE: Failed attempts include the following:
- The athlete cannot touch their foot down on the floor before returning back to the starting position. Any loss of balance will result in a failed attempt.
- The athlete cannot hold onto any implement to aid their balance.
- The athlete must keep their hands on their hips at all times throughout the test.
- The athlete must lightly touch their toe on the reach line whilst staying in full control of their body. Any loss of balance resulting in a heavy toe/foot contact with the floor should be regarded as a failed attempt.
With the test complete and all performances measured and recorded, the test administrator can then calculate the athlete’s SEBT performance scores using the following simple equations (17):
- Average distance in each direction (cm) = Reach 1 + Reach 2 + Reach 3 / 3
- Relative (normalised) distance in each direction (%) = Average distance in each direction / leg length * 100
These calculations should be performed for both the right and left leg in each direction, providing you with a total of 16 scores per athlete.
Though no validity coefficients are available for the SEBT, authors (23) have provided evidence that the SEBT is sensitive for screening various musculoskeletal injuries (17). Furthermore, high intratester reliability has been found for the SEBT (intraclass correlation coefficients = 0.78 – 0.96) (24).
We suggest you now check out this article on The Landing Error Scoring System (LESS).
All information provided in this article is for informational and educational purposes only. We do not accept any responsibility for the administration or provision of any testing conducted, whether that results in any positive or negative consequences. As an example, we do not take any responsibility for any injury or illness caused during any test administration. All information is provided on an as-is basis.
- Nelson, Brian D., “Using the Star Excursion Balance test as a predictor of lower extremity injury among high school basketball athletes” (2012).Theses and Dissertations. Paper 389. [Link]
- Gribble PA, Kelly SE, Refshauge KM, Hiller CE. Interrater Reliability of the Star Excursion Balance Test. Journal of Athletic Training 2013;48(5):621–626. [PubMed]
- Akbari M, Karimi H, Farahini H, Faghihzadeh S. Balance problems after unilateral lateral ankle sprains. J Rehabil Res Dev. 2006;43(7): 819–824. [PubMed]
- Gribble PA, Hertel J, Denegar CR. Chronic ankle instability and fatigue create proximal joint alterations during performance of the Star Excursion Balance Test. Int J Sports Med. 2007;28(3):236–242. [PubMed]
- Gribble PA, Hertel J, Denegar CR, Buckley WE. The effects of fatigue and chronic ankle instability on dynamic postural control. J Athl Train. 2004;39(4):321–329. [PubMed]
- Hale SA, Hertel J, Olmsted-Kramer LC. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J Orthop Sport Phys Ther. 2007;37(6):303–311. [PubMed]
- Hertel J, Braham RA, Hale SA, Olmsted-Kramer LC. Simplifying the Star Excursion Balance Test: analyses of subjects with and without chronic ankle instability. J Orthop Sport Phys Ther. 2006;36(3):131– 137. [PubMed]
- Martinez-Ramirez A, Lecumberri P, Gomez M, Izquierdo M. Wavelet analysis based on time-frequency information discriminate chronic ankle instability. Clin Biomech (Bristol, Avon). 2010;25(3): 256–264. [PubMed]
- Nakagawa L, Hoffman M. Performance in static, dynamic, and clinical tests of postural control in individuals with recurrent ankle sprains. J Sport Rehabil. 2004;13(3):255–268. [Link]
- Olmsted LC, Carcia CR, Hertel J, Shultz SJ. Efficacy of the Star Excursion Balance Tests in detecting reach deficits in subjects with chronic ankle instability. J Athl Train. 2002;37(4):501–506. [PubMed]
- Aminaka N, Gribble PA. Patellar taping, patellofemoral pain syndrome, lower extremity kinematics, and dynamic postural control. J Athl Train. 2008;43(1):21–28. [PubMed]
- Herrington L, Hatcher J, Hatcher A, McNicholas M. A comparison of Star Excursion Balance Test reach distances between ACL deficient patients and asymptomatic controls. Knee. 2009;16(2):149–152. [PubMed]
- McKeon PO, Ingersoll CD, Kerrigan DC, Saliba E, Bennett BC, Hertel J. Balance training improves function and postural control in those with chronic ankle instability. Med Sci Sports Exerc. 2008; 40(10):1810–1819. [PubMed]
- McLeod TC, Armstrong T, Miller M, Sauers JL. Balance improvements in female high school basketball players after a 6- week neuromuscular-training program. J Sport Rehabil. 2009;18(4): 465–481. [PubMed]
- Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36(12):911–919. [PubMed]
- Butler RJ, Lehr ME, Fink ML, Kiesel KB, Plisky PJ. Dynamic balance performance and noncontact lower extremity injury in college football players: an initial study. Sports Health. 2013;5(5): 417–422. [PubMed]
- Bressel E, Yonker JC, Kras J, Heath EM. Comparison of Static and Dynamic Balance in Female Collegiate Soccer, Basketball, and Gymnastics Athletes. Journal of Athletic Training 2007;42(1):42–46. [PubMed]
- Winter DA, Patla AE, Frank JS. Assessment of balance control in humans. Med Prog Technol. 1990;16:31–51. [PubMed]
- Zazulak B, Cholewicki J, and Reeves NP. Neuromuscular control of trunk stability: Clinical implications for sports injury prevention. J Am Acad Orthop Surg 16: 497–505, 2008. [PubMed]
- de Noronha M, Franca LC, Haupenthal A, Nunes GS. Intrinsic predictive factors for ankle sprain in active university students: a prospective study [published online January 20, 2012]. Scan J Med Sci Sports. doi:10.1111/j.1600-0838.2011.01434. [PubMed]
- McGuine T. Sports injuries in high school athletes: a review of injury-risk and injury-prevention research. Clin J Sports Med. 2006;16:488-499. [PubMed]
- Shaffer SW, Teyhen DS, Lorenson CL, Warren RL, Koreerat CM, Straseske CA, Childs JD. Y-Balance Test: a reliability study involving multiple raters. Mil Med. 2013;178(11):1264-70. [PubMed]
- Olmstead L, Carcia C, Hertel J, Shultz S. Efficacy of star excursion balance test in detecting reach deficits in subjects with chronic ankle instability. Journal of Athletic Training. 2002;37(4):501-507. [PubMed]
- Hertel J, Miller S, Denegar C. Intratester and intertester reliability during the star excursion balance test. Journal of Sport Rehabilitation. 2000;9(1):104-116. [Link]

Access our course on Agility for FREE!
Learn how to improve your athletes' agility. This free course also includes a practical coaching guide to help you design and deliver your own fun and engaging agility sessions.
Owen Walker
Owen is the Founder of Science for Sport and has a Master’s degree in Strength & Conditioning and a Bachelor’s degree in Sports Conditioning & Rehabilitation from Cardiff Metropolitan University. Before founding Science for Sport, he was the Head of Academy Sports Science at Cardiff City Football Club, and an interim Sports Scientist for the Welsh Football Association.
He’s published research on the ‘Practical Applications of Water Immersion Recovery Modalities for Team Sports’ in the Strength & Conditioning Journal by the NSCA (National Strength & Conditioning Association). He has also been featured in the Sports Business Journal and The Roar, Australia’s leading sports opinion website.
Learn from a world-class coach how you can improve your athletes' agility. This course also includes a practical coaching guide to help you to design and deliver your own fun and engaging agility sessions.

Why we exist
Our mission is to improve the performance of athletes and teams around the world by simplifying sports science and making it practical.
Try out our Academy and access our growing library of sports science courses.
Pricing FAQs Reviews Free trial
Get involved
Write for us Join our team
Blog Courses Newsletter Community Podcast Tools
About us Contact us Privacy policy Terms of use Terms and conditions Disclaimer
© 2024 Science for Sport | Catapult Sports
134k followers
13k followers
290k followers
826k followers
Star Excursion Balance Test | Postural Control | Return to Play

- Assessment E-Book
The Star Excursion Balance Test, abbreviated as SEBT consists of a series of reaching tasks with the lower extremity in eight directions. According to a study by Gribble et al. (2013) , the SEBT has excellent inter-rater reliability between 0.86 to 0.92 and has been shown to be able to differentiate individuals with lower limb conditions like chronic ankle instability, Patellofemoral pain, and ACL reconstructions. For this reason, we consider the SEBT as a test with a high clinical value in practice.
In order to conduct the test, first, place 6 strips of tape on the ground at an angle of 45°. Before the actual test is started, 4-6 practice trials in each direction are required after which your patient can rest for 5 minutes.
For the actual test, the patient has 3 official measured test moments. To start, have your patient stand barefoot on one limb with his hands on the hips and ask him to try to reach as far as possible along with each tape. The tape measure should be touched lightly with the most distal portion of the reaching foot without shifting weight to or coming to rest on the foot of the reaching limb and the examiner marks the most distal point of contact on the measuring tape.
A trial is not considered complete if the participant touched heavily, came to rest at touchdown, had to make contact with the ground with the reaching foot to maintain balance, or lifted or shifted any part of the foot of the stance limb during the trial.
After each a trial in a direction, the patient returns his reaching limb to the starting position at the apex of the grid resuming a bilateral stance again. Then, repeat the same procedure with the same limb in another direction. A full circuit is done for one limb if all directions have been covered. Then switch legs and complete another full circuit. At the end of the Star Excursion Balance Test, the patient should have completed 3 full circuits with both legs and the distance of each trial should be measured.
Scoring: To score the SEBT, first calculate the average reach distance in each direction in centimeters, by dividing the sum of all 3 trials per leg through 3. So you should have 16 values. Then, calculate the relative (or normalized) distance in each direction as a percentage by taking the average distance in each direction, divided by the patient’s leg length, and multiplied by 100. If you now compare the legs with each other, this enables you to identify athletes with a higher risk of injury. For example, Plisky et al. (2006) found that an anterior reach asymmetry of greater than 4cm during the SEBT predicted individuals at higher risk for lower limb injuries in basketball players.
Pollock et al. (2010) found that Collegiate American football players with a composite score of less than 90% are 3.5 times more likely to sustain an injury.
Of course, these are only samples of two sport-specific cohorts which is why it is important to mention that the application and the generalization of the SEBT should be carefully considered for each sport and sex, as there is a huge variance in SEBT performance and injury risk between sports and sexes!
LEARN TO OPTIMIZE REHAB & RTS DECISION MAKING AFTER ACL RECONSTRUCTION

Other useful performance tests that you might be interested in are:
- Y-Balance Test
- Drop Jump Test
- Hop Test Cluster
Butler RJ, Lehr ME, Fink ML, Kiesel KB, Plisky PJ. Dynamic balance performance and noncontact lower extremity injury in college football players: an initial study. Sports health. 2013 Sep;5(5):417-22.
Bressel E, Yonker JC, Kras J, Heath EM. Comparison of static and dynamic balance in female collegiate soccer, basketball, and gymnastics athletes. Journal of athletic training. 2007 Jan;42(1):42.
Gribble PA, Kelly SE, Refshauge KM, Hiller CE. Interrater reliability of the star excursion balance test. Journal of athletic training. 2013;48(5):621-6.
Hubbard TJ, Kramer LC, Denegar CR, Hertel J. Contributing factors to chronic ankle instability. Foot & ankle international. 2007 Mar;28(3):343-54.
Plisky PJ, Gorman PP, Butler RJ, Kiesel KB, Underwood FB, Elkins B. The reliability of an instrumented device for measuring components of the star excursion balance test. North American journal of sports physical therapy: NAJSPT. 2009 May;4(2):92.
Robinson RH, Gribble PA. Support for a reduction in the number of trials needed for the star excursion balance test. Archives of physical medicine and rehabilitation. 2008 Feb 1;89(2):364-70.
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Become an ACL rehab specialist in this world class online course and nail your patient's return-to-sport!

What customers have to say about this online course

Create your free account to gain access to this exclusive content and more!
To provide the best experiences, we and our partners use technologies like cookies to store and/or access device information. Consenting to these technologies will allow us and our partners to process personal data such as browsing behavior or unique IDs on this site and show (non-) personalized ads. Not consenting or withdrawing consent, may adversely affect certain features and functions.
Click below to consent to the above or make granular choices. Your choices will be applied to this site only. You can change your settings at any time, including withdrawing your consent, by using the toggles on the Cookie Policy, or by clicking on the manage consent button at the bottom of the screen.
Download our free physiotherapy app with all the knowledge you need.

Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

The Star Excursion Balance Test: An Update Review and Practical Guidelines

2021, International Journal of Athletic Therapy and Training
The Star Excursion Balance Test (SEBT) is a reliable, responsive, and clinically relevant functional assessment of lower limbs’ dynamic postural control. However, great disparity exists regarding its methodology and the reported outcomes. Large and specific databases from various population (sport, age, and gender) are needed to help clinicians when interpreting SEBT performances in daily practice. Several contributors to SEBT performances in each direction were recently highlighted. The purpose of this clinical commentary is to (a) provide an updated review of the design, implementation, and interpretation of the SEBT and (b) propose guidelines to standardize SEBT procedures for better comparisons across studies.
Related Papers
Physical education of students
Background and Study Aim: Balance control has been regarded as a crucial factor in sports and indicated as an important element to be examined for the risks of injury. But it is unknown whether the dynamic balance changes according to the player positions in professional soccer players. To determine whether there were differences in the dynamic balance performance of the different positions of Turkish professional soccer players from within one squad. Material and Methods: Twenty-four professional soccer players were divided into 4 groups by the coach, including goalkeepers (n = 3), midfielders (n = 6), defenders (n = 7) and forwards (n = 8). Prior the competition season, anthropometric characteristics of players were measured. Then, players were tested Y Balance Test (YBT) for the anterior (ANT), posteromedial (PM), and posterolateral (PL) reach distances and limb lengths bilaterally. Results: The goalkeepers were heavier compared with the midfielders. Furthermore, the BMI of the g...
Physical Treatments: Specific Physical Therapy Journal (PTJ)
Purpose: Recently, the Functional Movement Screen (FMS) and Y Balance Tests are used to assess the key movement patterns, dynamic stability and to identify individuals at high risk of injury. But, there are few studies to assess the relationship between the FMS test and Y Balance Test. This study aimed to assess the relationship between dynamic stability and the FMS test. Methods: The subjects of this study were 95 students (Mean±SD age=26.7±3.13 y, Mean±SD height=177.4±6.9 cm, Mean±SD weight=72.02±6.91 kg, and Mean±SD BMI=22.93±0.41 kg/ m2) from a university complex. All subjects were evaluated prior to the onset of training. Y Balance Test was used to evaluate dynamic stability and FMS test for evaluating the movement patterns of the subjects. Results: The Pearson correlation coefficient was used to assess the relationship between variables. The results showed a significant association between the FMS score and the aggregate Y score (r=0.205, P=0.04). Also, there was a weak correlation between FMS and normalized posteromedial reach (r=0.27, P=0.04). However, the correlation between FMS and normalized anterior reach and posterolateral reach was not statistically significant (P>0.05). Conclusion: These findings demonstrate partial correspondence between the two tests. However, the relationship is not strong enough to consider them interchangeable. Thus, dynamic postural control is not a large component of the aggregate FMS score.
Journal of Functional Morphology and Kinesiology
Dynamic postural control is challenged during many actions in sport such as when landing or cutting. A decrease of dynamic postural control is one possible risk factor for non-contact injuries. Moreover, these injuries mainly occur under loading conditions. Hence, to assess an athlete’s injury risk properly, it is essential to know how dynamic postural control is influenced by physical load. Therefore, the study’s objective was to examine the influence of maximal anaerobic load on dynamic postural control. Sixty-four sport students (32 males and 32 females, age: 24.11 ± 2.42, height: 175.53 ± 8.17 cm, weight: 67.16 ± 10.08 kg) were tested with the Y-Balance Test before and after a Wingate Anaerobic Test on a bicycle ergometer. In both legs, reach distances (anterior) and composite scores were statistically significantly reduced immediately after the loading protocol. The values almost returned to pre-load levels in about 20 min post-load. Overall, findings indicate an acute negative...
International Journal of Sports Physical Therapy
Brice PICOT
Background Lower extremity injuries among young female handball players are very common. The modified Star Excursion Balance Test (mSEBT) is a valid clinical tool to assess dynamic postural control and identify athletes with higher risk of injury. However, its interpretation is difficult since performance on this test is highly sport dependent. No normative values on the mSEBT exist in handball. Purpose The aim of this investigation was to establish normative ranges of mSEBT performance in young, healthy female handball players to help practitioners when interpreting risk estimates. Study design Cross-Sectional Study Methods Athletes from 14 elite teams were recruited during a national tournament and performed 3 trials in the anterior (ANT), posteromedial (PM), posterolateral (PL) directions of the mSEBT. Means, standard deviations and 95% confidence intervals (95%CI) of normalized reached distances were calculated for each direction and the composite score (COMP). Level of asymmetr...
Ariel S Mandelblum
Humans are creatures of habit, and once the chain has been severed, our routines become horribly disrupted affecting every large & small detail of our lives. Injuries affect both the body and the mind, and without one, the other cannot thrive or hope to recover. Identified on this board are four of the most commonly known postural control assessments, as well as can be utilized to identify injuries as a means of pre-participation screening for athletes. The NCAA (National Collegiate Athletic Association), along with sports psychologists attest to the notion of training the mind even if the body cannot due to an injury. The purpose of this report is to identify which of the four examination protocols presents the highest degree of reliability, and validity towards identifying lower extremity injuries (ankle, knee, hip).
Riley Kenney
Kenney, Riley, MAT, May 2017 Athletic Training REVIEWING THE USE OF INJURY SCREENING ASSESSMENTS AND IDENTIFYING RISK OF INJURY Lower extremity injures account for over half of reported sports related injuries with the ankle and knee being the most commonly injured joints. The majority of non-contact injuries related to these two joints can potentially be prevented through individualized prevention programs. Biomechanical injury screening has the potential to identify the risk factors associated with injury and allows the implementation of targeted rehabilitation strategies to combat the identified deficits. There is substantial need for screening assessments that are practical and accurate for the clinical athletic trainer. This literature reviewed examined the dorsiflexion lunge test, Functional Movement Screen (FMS), Y-Balance, Star Excursion Balance Test and the lower extremity strength assessment as preseason screening tools and their ability to predict future injury of primari...
Dr. YOUSEF ALSHEHRE , Khalid Alkhathami
Background: Individuals with chronic low back pain (CLBP) may demonstrate reduced ability to perform dynamic tasks due to fear of additional pain and injury in response to the movement. The Y-balance test (YBT) is a functional and inexpensive test used with various populations. However, the reliability and validity of the YBT used for assessing dynamic balance in young adults with CLBP have not yet been examined. Purpose: To determine the inter-rater reliability of the YBT and to compare dynamic balance between young adults with CLBP and an asymptomatic group. Study Design: Reliability and validity study. Methods: Fifteen individuals with CLBP (≥ 12 weeks) and 15 age- and gender-matched asymptomatic adults completed the study. Each group consisted of 6 males and 9 females who were 21-38 years of age (27.47 ± 5.0 years). The YBT was used to measure participant’s dynamic balance in the anterior (ANT), posteromedial (PM) and posterolateral (PL) reach directions. The scores for each participant were independently determined and recorded to the nearest centimeter by two raters. Both the YBT reach distances and composite scores were collected from the dominant leg of asymptomatic individuals and the involved side of participants with CLBP and were used for statistical analysis. Results: The YBT demonstrated excellent inter-rater reliability, with intraclass correlation coefficients ranging from 0.99 to 1.0 for the YBT scores of both asymptomatic and CLBP groups. The CLBP group had lower scores than those of the asymptomatic group in the reach distances of the ANT (p = 0.023), PM (p < 0.001), and PL (p = 0.001) directions, and the composite scores (p < 0.001). Conclusions: The results demonstrated excellent inter-rater reliability and validity of the YBT for assessing dynamic balance in the CLBP population. The YBT may be a useful tool for clinicians to assess dynamic balance deficits in patients with CLBP.
The Journal of orthopaedic and sports physical therapy
Cailbhe Doherty
Study Design Controlled laboratory study. Objective To utilize kinematic and stabilometric measures to compare dynamic balance during performance of the Star Excursion Balance Test (SEBT) between persons 6-months post first-time lateral ankle sprain (LAS) and a non-injured control group. Background Biomechanical evaluation of dynamic balance in persons following first-time LAS during SEBT performance could provide insight into the mechanism(s) by which individuals proceed to recover fully, or develop chronic ankle instability. Methods Sagittal-plane kinematics of the lower extremity and the center of pressure (COP) path during the performance of the anterior (ANT), posterior-lateral (PL) and posterior-medial (PM) reach directions of the SEBT were obtained from 69 participants, 6 months following first-time acute LAS. Data also were obtained from 20 non-injured controls. Results The LAS group displayed lower normalized reach distances in all 3 reach directions compared to control par...
German Journal of Exercise and Sport Research
Dynamic postural control is one of the essential factors in situations where non-contact injuries mainly occur, i.e., landing, cutting, or stopping. Therefore, testing of dynamic postural control should be implemented in injury risk assessment. Moreover, non-contact injuries mainly occur under loaded conditions when the athlete is physically stressed. Therefore, risk factors and mechanisms of these injuries should also be regarded under loading conditions and not only when the athlete is recovered. Current studies examining the influence of physical load on risk factors, such as dynamic postural control, often use cycling protocols to stress the participants. Nevertheless, most types of sports require running as a central element and the induced internal load after cycling might not be the same after running. Therefore, the current study aimed to examine the influence of a running and a cycling protocol on dynamic postural control and to determine the potential injury risk under rep...
Journal of sport rehabilitation
Mary Ireland
The Y-Balance Test was developed as a test of dynamic postural control and has been shown to be predictive of lower extremity injury. However, the relationship between hip strength and performance on the Y-Balance Test has not been fully elucidated. The goal of this study was to identify the relationship between components of isometric hip strength and the Y-Balance Test, to provide clinicians better guidance as to specific areas of muscle performance to address in the event of poor performance on the Y-Balance Test. Laboratory Study. Biomechanics Laboratory. Seventy-three healthy participants, 40 males and 33 females, volunteered for this study. None. Participants completed the Y-Balance Test on the right leg. We then measured peak isometric torque in hip external rotation, abduction, and extension. Correlations were calculated between torque measurements, normalized for mass, and Y-Balance Test performance. Significant relationships were used in linear regression models to determi...
RELATED PAPERS
Journal of Orthopaedic & Sports Physical Therapy
Timothy Hewett
Journal of athletic training
Conor Gissane
IJAR Indexing
Acta of bioengineering and biomechanics
Katarzyna Walaszek
Technology and Health Care
Agnė Slapšinskaitė-Dackevičienė
Physical Treatments: Specific Physical Therapy
Niloofar Mohammadi
Journal of Sport Rehabilitation
Monna Arvinen-Barrow
Asian Journal of Sports Medicine
Marcelo Coertjens
Hélène Moffet
behnaz ganji
Archives of Physiotherapy
Jo Verschueren
Brain and Behavior
International journal of sports physical therapy
Robin Queen
Sports biomechanics / International Society of Biomechanics in Sports
Francesco Travascio
Gait & Posture
Daniel Hamacher
David F Stodden
Journal of Athletic Training
Kathryn Refshauge
International Journal of Environmental Research and Public Health
Ahmad Alghadir
Iranian Rehabilitation Journal
Nastaran Ghotbi
Fisioterapia em Movimento
Víctor Salinas Palacios
Physiotherapy Research International
Andrés Pierobon
Iranian Rehabilitation Journal (IRJ) , Nastaran Ghotbi
Turkiye Klinikleri Journal of Health Sciences
Logan Ruhde
Amir Sarshin
Biology of Exercise
Ertugrul YUKSEL
Journal of Sports Sciences
Sports Health: A Multidisciplinary Approach
Kyle Kiesel
https://www.ijrrjournal.com/IJRR_Vol.7_Issue.8_Aug2020/Abstract_IJRR0022.html
International Journal of Research & Review (IJRR)
Journal of Science and Medicine in Sport
Phillip Gribble
Malaysian Journal of Medical Sciences
Kanok-on Thanasootr
IOSR Journals
Ege Tıp Bilimleri Dergisi
Physical Treatments - Specific Physical Therapy
Behnaz Ganji
Lucas Correa
Physiotherapy Practice and Research
Jim Richards
mostafa zarei
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024

Star Excursion Balance Test
My favourite dynamic postural control objective outcome measure.
Firstly, thanks for checking out the video. I hope that it was helpful and if you are not already using the Star Excursion Balance Test you will now. This is the information that I felt was too ‘nitty gritty’ to include in the video.
Reliability of the Star Excursion Balance Test
The reliability of the SEBT components utilised (i.e. the anterior, posteromedial and posterolateral) ranged from 0.82 to 0.87 (ICC3,1) (Plisky et al. 2006). To put this in perspective, it is of similar reliability to assessing knee flexion ROM with a universal goniometer (Brosseau et al. 1997).
Clinical Implications of This Measure
Assessing Intervention Effectiveness: as a reliable measure, you can use it to gauge an athletes improvements in dynamic postural control over time.
Injury Prediction: Plisky et al. (2006) showed that athletes with anterior left/right reach differences greater than 4 cm were 2.5 times more likely to sustain a lower limb injury over the course of a season. They also found that female athletes with a composite reach distance less than 94.0% of their limb length (measured from ASIS to lateral malleolus) were 6.5 times more likely to have a lower extremity injury!
Relevant to Athletic Population: the SEBT is sensitive enough to show dynamic postural control in a number of athletic populations including ACL deficient and Chronic Ankle Instability patients (Herrington et al. 2009; Hertel et al. 2006).
Conclusions
My conclusion is that is a sweet test. If you want to objectively assess an athlete’s responses to neuromuscular and postural control training (and honestly why would you not) this is your go-to. This can be a massive motivational tool, and also proves how helpful your exercises are. Also, if you want to “pre-screen” for injury this can also be used as a helpful predictor and should be a component of your assessment.
Go set it up right now, and enjoy your new favourite outcome measure.
Brosseau L, Tousignant M, Budd J, Chartier N, Duciaume L, Plamondon S, O’Sullivan JP, O’Donoghue S, Balmer S. Intratester and intertester reliability and criterion validity of the parallelogram and universal goniometers for active knee flexion in healthy subjects. Physiotherapy Research International 1997; 2(3):150-166
Herrington L, Hatcher J, Hatcher A, McNicholas M. A comparison of Star Excursion Balance Test reach distances between ACL defiient patients and asymptomatic controls. The Knee 16 (2009) 149–152
Hertel J, Braham RA, Hale SA, Olmsted Kramer LC. Simplifying the Star Excursion Balance Test: Analyses of Subjects With and Without Chronic Ankle Instability. J Orthop Sports Phys Ther 2006;36:131-137.
Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a Predictor of Lower Extremity Injury in High School Basketball Players. J Orthop Sports Phys Ther 2006;36(12):911-919
Related Posts
hey fellow profession,
im a brazilian academic of physiotherapy and my work of completion of course is about a star test balance in injury of ACL and I don’t have found articles about SEBT, so you can send me your references on this post???
i really need… thanks
Natália Goulart ( [email protected] )
Hi Natália,
Thanks for your interest. Unfortunately, I am not able to distribute PDF documents of articles given this is digital piracy. You can, however, access these articles via each Journal’s website e.g. Journal of Orthopaedic Sports and Physical Therapy: http://www.jospt.org/ .
Hope this helps you out!
I currently using SEBT for my dissertation and I am at the point of putting the results into microsoft excel. What I wanted to know was what is the correct equation for measuring the composite scores?
Hope you can answer this Thanks
Seti ( [email protected] )
[…] This post was mentioned on Twitter by The Sports PT, The Sports PT. The Sports PT said: My favourite dynamic postural control measure – The Star Excursion Balance Test. http://bit.ly/9Eo7GN #physiotherapy #physicaltherapy […]
- MMT Online Seminar
- MMT Insiders

- Online Mentoring
- Top Products
Star Excursion Balance Test & Dynamic Postural Control
- Anterior (ANT), posteromedial (PM) and posterolateral (PL) lines.
- Stand on the central point.
- Hands on hips.
- Reach as far as you can along the line and gently tap the line.
- Do not come to rest on the line.
- Do not transfer your body weight onto the reaching leg.
FACTORS AFFECTING PERFORMANCE
- Vastus medialis is most active in anterior reach.
- Vastus lateralis is least active in lateral reach.
- Medial hamstring is most active during anterolateral reach.
- Bicep femoris was most active during posterior and posterolateral reach.
WHAT DOES THE SEBT TELL US?
Chronic ankle instability (cai):.
- In CAI, all three directions have the ability to identify reach deficits in participants compared to healthy controls, however, the PM is the most representative of the overall performance (Hertel, Braham, Hale & Olmsted-Kramer., 2006).
- Anterior reach is more impacted by dorsiflexion ROM and plantar cutaneous sensation, meaning that mechanical restrictions and sensory deficits impact this movement.
- DF ROM is best evaluated with the knee to wall weight bearing lunge test compared to non weight bearing AROM (Dill et al., 2014).
- Posteromedial and posterolateral reach is more impacted by eversion strength and balance control.
- De la Motte, Arnold & Ross (2015) studied the movement pattern differences in trunk rotation and found that patients with CAI are more likely to use increased trunk flexion during anterior reach which suggests a compensation strategy for reduced ankle control is to manipulate the pelvis and trunk.
ANTERIOR CRUCIATE LIGAMENT RECONSTRUCTION (ACLR):
- The same authors (De la Motte, Arnold & Ross., 2015, p.358) also studied trunk movements in ACL patients and found that following an ACLR, when reaching forward, patients are more likely to rotate their trunk away (backwards) from the reach leg and externally rotate the pelvis on the stance leg.
- In a different study following ACLR, researchers found that when looking above the ankle and at the knee, patients with reduced quadricep strength have reduced reach capacity in the anterior directions (Clagg, Daterno, Hewett & Schmitt., 2015).
- These same authors also found that hip abductions strength impacts all 3 directions, telling us that dynamic balance has contributions from the foot, ankle, knee, hip and trunk and our assessment of movement patterns should try consider all these areas too.
PATELLOFEMORAL PAIN SYNDROME (PFPS):
IMPLEMENTATION INTO REHAB


REFERENCES:

Erson Religioso III, DPT, FAAOMPT
Post a comment, become a tmj/headache speciliast.

Eval, Reset, and Stabilize System

Get Certified in BFR Online!
Search for jobs.

IASTM Technique 2.0

EDGE Restriction System BFR Cuffs

Knee Rehab Done Right
Google workspace for emr.

Modern Manual Therapy Insiders
Featured Post
How to explain sij pain without using sij, rotation, or innominate.
One of the most frequently asked questions I get at Modern Manual Therapy courses is, "How do you explain SIJ dysfunction without us...
Total Pageviews
Blog archive.
- Dr. E's Private Network
- Dr. E's Shop
- Modern Manual Therapy
- EDGE Rehab and Sport Science
- Online Seminars
Unlimited CEUs

CashPT Blueprint

Copyright © 2023
Copyright 2015 Modern Manual Therapy Blog - Manual Therapy, Videos, Neurodynamics, Podcasts, Research Reviews | Designed by Veethemes.com

Star Excursion Balance Test (SEBT)
Table of Contents
What is a Star Excursion Balance Test (SEBT)?
The Star Excursion Balance Test (SEBT) is a dynamic balance test that measures the ability of an individual to reach out and touch a target with one foot while balancing on the other foot. The test is performed on a grid with eight lines radiating from a central point, each line representing a different direction.
The participant stands on one foot in the center of the grid and reaches out as far as possible along each line, with their hands on their hips. The distance that the participant can reach is measured and recorded.
The SEBT is a reliable and valid measure of dynamic balance, and it has been shown to be a good predictor of lower extremity injury risk. The test is also sensitive to changes in balance following injury or rehabilitation .
- To assess dynamic balance, which is the ability to maintain stability while moving.
- Identifying athletes at risk for injury
- Monitoring progress during rehabilitation
- Screening for balance deficits and core control
Equipment required:
Measuring tape, marking tape, and a flat, non-slippery surface. Four 120 cm pieces of marking tape have been set out on the ground before the test, intersecting in the middle, with the lines drawn at 45° angles.
Preparations:
To the subject, explain the test methods. Carry out the necessary warm-up.
Technique of Star Excursion Balance Test
The SEBT’s objective is to keep one leg in a single-leg stance while reaching the opposing leg as far as feasible.
The participant stands barefoot on one foot in the center of the grid. The participant reaches out as far as possible along each line, with their hands on their hips. The test subject is required to balance on one leg while spreading the other leg as far as they can in eight different directions. The participant must reach in 8 distinct positions, once in each of the following directions: anterior, anteromedial, medial, posteromedial, posterior, posterolateral, lateral, and anterolateral (for example, when standing on his or her left leg). The distance that the participant can reach is measured and recorded. The participant repeats the test on the other foot. The average reach distance for each direction is calculated for both feet. Athletes who are more likely to sustain lower extremity injuries and people with chronic ankle instability may be better identified using the anterior, posteromedial, and posterolateral positions.
When the subject exhibits a significantly shorter reach while standing on the injured limb compared to while standing on the healthy leg, SEBT has demonstrated the subject’s lack of dynamic postural control.
A factor analysis revealed that one reach direction in particular (posteromedial) was able to effectively identify people with chronic ankle instability as well as performing all eight directions. The test originally included reaching in eight directions while standing on each foot.
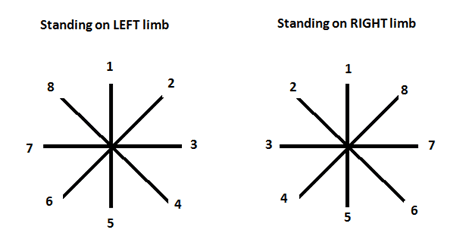
8 Directions are:
- Anteromedial
- Posteromedial
- Posterolateral
- Anterolateral
Star Excursion Balance Test (SEBT) Video
The ‘Y-test’ is a test that is comparable to the SEBT but uses only three directions.
Scoring System of Star Excursion Balance Test
All distances reached during the test are recorded to the closest 0.5 cm. Calculate the average of the three measurements for each direction, as well as the relative distance in each direction (normalized) (%) (average distance in each direction/leg length * 100).
Average distance in each direction (cm):
Reach 1 + Reach 2 + Reach 3 / 3
Relative (normalized) distance in each direction (%):
Average distance in each direction/leg length*100
These calculations should be made for the right and left legs in both directions, giving each athlete a total of 16 scores.
Star Excursion Balance Test normal values
Age, sex, and sport all affect the Star Excursion Balance Test (SEBT) normal values. The relative reach distance in each direction should, however, generally be larger than 85% of the leg length.
Here are a few examples of typical SEBT values for various populations:
Healthy Young Adults:
- Anterior reach: 94-100% leg length
- Posteromedial reach: 91-100% leg length
- Posterolateral reach: 70-94% leg length
- Anterior reach: 100-105% leg length
- Posteromedial reach: 95-105% leg length
- Posterolateral reach: 75-100% leg length
Older adults :
- Anterior reach: 85-95% leg length
- Posteromedial reach: 80-90% leg length
- Posterolateral reach: 65-85% leg length
It is important to note that these are only general guidelines. Speak with your doctor or physical therapist to find out what is typical for you. They can administer the SEBT and compare your results to those of individuals with similar ages and levels of activity.
It’s not always a sign of a problem if your SEBT score is below average. However, it can indicate that your risk of injury has increased. You can create a strategy to increase your balance and lower your risk of injury with the assistance of your physician or physical therapist.
Advantages:
This test can be carried out easily and cheaply with basic tools.
Disadvantages:
If the test needs to be run on a large number of people, it can take some time.
- Hertel, Miller, and Deneger (2000) claim that r = 0.85-0.96 represents the reliability of the SEBT.
- Plisky et al. (2006) report that this test’s reliability varies between 0.82 to 0.87, scoring 0.99 for the measurement of limb length.
- Another study found: According to Hardy et al. (2008), intra-class correlation coefficients for the SEBT’s reliability ranged from 0.67 to 0.87.
- According to Chaiwanichsiri et al. (2005), the Star Excursion Balance training was superior to a traditional rehabilitation program in terms of enhancing the functional stability of an ankle that had been injured.
- According to Plisky et al. (2009), the SEBT’s intra-rater reliability is moderate to good (ICC 0.67–0.97) and its inter-rater reliability is poor to good (0.35-0.93).
When comparing reach deficits between and within participants with unilateral chronic ankle instability , the SEBT seems to be an effective method.
Additionally, it can be applied to identify weaknesses and asymmetries in people and support the decision-making process for a return to play.
Why is Balance important in sports?
Balance also referred to as “postural control,” can be described statically as the capacity to hold oneself steady while making only minimal movements, and dynamically as the capacity to carry out an action while holding a steady stance. The capacity to hold a stable position in a fast-paced sporting situation is essential for both effective application of the talent and lowering the risk of harm.
Testing and tracking an athlete’s dynamic stability may be very important since dynamic balance is an essential component of performance and because having poor balance is associated with a higher risk of injury.
Dynamic balance can be measured with accuracy and validity using the Star Excursion Balance Test (SEBT). It has been shown to be a good predictor of lower extremity injury risk, and it is sensitive to changes in balance following injury or rehabilitation.
Athletes, people who have had injuries to their lower extremities, and older people can all be assessed for dynamic balance with the SEBT. The test can be used to check for balance issues, identify athletes who are vulnerable to injuries, and track improvement throughout recovery.
Star Excursion Balance Test. (n.d.). Physiopedia. https://www.physio-pedia.com/Star_Excursion_Balance_Test Star Excursion Balance Test -. (2017, December 3). https://exercise.trekeducation.org/assessment/balance-testing/star-excursion-balance-test/ Walker, O. (2023, August 31). Star Excursion Balance Test. Science for Sport. https://www.scienceforsport.com/star-excursion-balance-test/ Star Excursion Balance Test. (n.d.). https://www.topendsports.com/testing/tests/balance-star-excursion.htm
Author: Nitesh Patel - Physiotherapist
Physiotherapist in Samarpan Physiotherapy Clinic Ahmedabad Bapunagar Amaraiwadi Vastral Mobile Physiotherapy Clinic Dr. Nitesh Patel ( Physiotherapist ) : Mo No : 09898607803
Similar Posts

Calf muscle pain
What is calf muscle pain? What calf pain feels like? Sing and symptoms of calf muscle pain Causes of calf muscle pain Calf pain may result from several different causes and can be associated with other health conditions. While you can often treat calf pain reception, other instances may require immediate medical attention.Here are some…
![star excursion balance test average Test for tight retinacular [ collateral ] ligaments:](https://mobilephysiotherapyclinic.in/wp-content/uploads/2022/02/test-for-tight-retinacular-ligaments.jpg)
Test for tight retinacular [ collateral ] ligaments:
This test is also known as the Harness – Zancolli test. This test is used to check the tightness of the retinacular ligaments. This clinical test is applied by the therapist when the patient is complain about the wrist joint. What is the purpose of the Test for tight retinacula [ collateral ] ligaments? This…

Thumb ulnar collateral ligament laxity test:
This thumb ulnar collateral ligament laxity test is also known as the thumb ulnar collateral ligament instability test. This thumb ulnar collateral ligament laxity test is applied to the clinic to check the tear of the collateral ligament. This thumb ulnar collateral ligament laxity test is applied by to physiotherapist when the patient is complaining…

Modified Ashworth Scale of Spasticity
Modified Ashworth Scale of Spasticity is a common scale to use for measuring spasticity in those with cerebral palsy, stroke, and other neurological disorders. The Modified Ashworth Scale is a scale that is used to quantify the amount of spasticity or stiffness in a patient. The Modified Ashworth Scale has five different symptom severity levels…

Special test for the plica of knee :
This all test is applied by to therapist & doctor for check to injury around to knee . It is apply into examination part of to assessment . thus test is help to doctor or therapist into diagnosis of the knee injury . What is plica of knee ? Into knee joint plica are embryological…

Sacroiliac rocking test:
This test is also known as the knee to shoulder test for SI joints. This test is called to sacrotuberous ligament stress test. This test is applied by the to clinic check the dysfunction of the sacroiliac joint. This clinical test is applied by to therapist when the patient is complaining about SI joint pain…
Leave a Reply Cancel reply
You must be logged in to post a comment.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Sports (Basel)
- PMC10383250
Star Excursion Balance Test as a Predictor of Musculoskeletal Injury and Lower Back Pain in Non-Professional Soccer Players
Iva sklempe kokic.
1 Faculty of Kinesiology, Josip Juraj Strossmayer University of Osijek, 31000 Osijek, Croatia; [email protected] (I.S.K.); rh.sofik@anukd (D.K.)
Katarina Petric
2 Faculty of Health Studies, University of Rijeka, 51000 Rijeka, Croatia; [email protected]
Danijela Kuna
Stjepan jelica.
3 Department of Health Studies, College of Applied Sciences, “Lavoslav Ruzicka” in Vukovar, 32000 Vukovar, Croatia; rh.uvev@acilejs
Tomislav Kokic
4 Faculty of Medicine, Josip Juraj Strossmayer University of Osijek, 31000 Osijek, Croatia
5 Department of Orthopaedics and Traumatology, County General Hospital Vinkovci, 32100 Vinkovci, Croatia
Associated Data
The data presented in this study are available on request from the corresponding author.
Soccer is a sport with worldwide popularity but has a substantial risk of injury. Clinical screening tools are an important factor in strategies of injury prevention. The purpose of the study was to examine the relationship between the Star Excursion Balance Test (SEBT) and injury and lower back pain (LBP) in amateur soccer players. The research was performed as a longitudinal cohort study on 42 amateur male soccer players with 15.8 ± 6.6 years of soccer playing (age: 25.5 ± 6 years). Participants were surveyed with regard to their soccer playing, injuries, and LBP, and the SEBT was performed. They were followed for 3.5 months. At the follow-up, an additional set of data regarding injuries and LBP was gathered. Significant differences were found in all directions and in the composite score of the SEBT between uninjured and injured players. Shorter distance in all directions and a lower composite score were associated with injury in general. Shorter distances in all but the anterior direction and a lower composite score were associated with lower extremity injury, and shorter anterior distance was associated with LBP. Amateur soccer players with lower SEBT scores are more prone to injuries in general, as well as injuries of the lower extremities. SEBT presents as a useful clinical screening tool in identifying amateur soccer players at risk of injury.
1. Introduction
Soccer is a sport with worldwide popularity; however, the risk of injuries during practice and the game is high. The incidence of injuries in amateur soccer players ranges from 2.7 to 4.5 per 1000 h of practice and from 12.3 to 24.7 per 1000 h of game time [ 1 , 2 , 3 ]. The majority of soccer related injuries (68–88%) occur in the lower extremities [ 4 , 5 ]. Lower back pain (LBP) is another very common musculoskeletal disorder in soccer players with a yearly prevalence of 64% [ 6 ]. Participation in soccer can also have a significant role in the development of strength asymmetries leading to injury occurrence [ 7 ].
Prevention of injuries has an important role in reducing the injury burden in non-professional soccer players [ 8 , 9 ]. The use of clinical screening tools became an important component in the prevention of sports injuries. Previous studies have suggested that the use of an injury-screening tool related to dynamic balance may be beneficial in the identification of the risk of injury [ 10 , 11 , 12 , 13 ]. Dynamic balance can be defined as an individual’s ability to maintain total body stability of their center of mass during movement and is an integral part of neuromuscular control [ 14 ]. Deficits in lower extremity dynamic neuromuscular control, including impaired dynamic balance, is a known risk factor for injury [ 13 , 15 , 16 ]. Furthermore, dynamic balance is also impaired in individuals with LBP [ 17 , 18 ]. Dynamic neuromuscular control is a frequently utilized component of injury prevention programs as well as an outcome measure for return to sport criterion [ 10 ].
There is the need to further establish the relationship between dynamic balance and the risk of musculoskeletal injury and LBP in the amateur athlete population and to assess whether a clinical screening test for dynamic balance can be useful in the prediction of injuries and LBP. A valid and reliable screening tool for dynamic balance could be used in identifying those at risk and in the planning of preventive strategies. One of the very common screening tools for dynamic balance is the Star Excursion Balance Test (SEBT) [ 13 , 19 ]. The SEBT evaluates dynamic postural stability [ 20 ]. It is an inexpensive, simple, and quick method of measuring dynamic balance with good reliability reported [ 19 , 21 ]. In addition to dynamic balance, SEBT also requires other characteristics of neuromuscular control, such as coordination, flexibility, and strength, and each reach direction activates muscles in a different pattern [ 13 , 22 ].
Previous studies reported that reach asymmetries in anterior, posteromedial, and posterolateral direction of ≥4 cm, a normalized composite score <89.6%, and shorter individual reach distances during the SEBT and modified SEBT were associated with future injury risk [ 10 , 16 ]. However, the majority of the studies were not performed on non-professional athletes. Current information regarding the predictive value of SEBT for musculoskeletal injury and LBP in amateur athletes is still limited.
Therefore, the purpose of this study was to examine the relationship between SEBT reach distances and musculoskeletal injury and LBP among non-professional soccer players. We hypothesized that the SEBT can be used in the prediction of musculoskeletal injury and LBP in this population, and that there will be significant associations between shorter reach distances and injuries and LBP.
2. Materials and Methods
2.1. study design and participants.
The study was performed as a longitudinal cohort study on 42 amateur male soccer players from three amateur soccer clubs in Eastern Croatia. All three soccer clubs are part of the regional league, and they compete at the regional level. Ethical approval for the study was obtained from the Ethics Committee for Biomedical Research, Faculty of Health Studies, University of Rijeka, Croatia (21 February 2019). The study was carried out in accordance with the Declaration of Helsinki and participants gave their written consent. The inclusion criteria for participants were as follows: amateur soccer player, regular practice and games in the soccer club for at least six months before the beginning of the study, and an active soccer player for at least 5 years. Exclusion criteria were injuries or painful symptoms in the period of performing the screening tests and any other serious medical conditions, including surgery or concussion, six months before the testing.
2.2. Procedures
Participants completed the questionnaire with the baseline information, which included demographic data, body height and body mass, health-related history, duration of soccer practice, training loads in the past six months, existence of injuries and lower back pain in the past six months, as well as leg dominance. Leg length was measured on each lower limb 3 times, from the greater trochanter to the lateral malleolus. Body mass index was obtained using the standard equation. After the initial interview, participants performed the SEBT after 10 min of warm up. Participants were followed up 3.5 months after the initial interview with another questionnaire, which included information on training loads, injuries, and lower back pain in the period after the initial interview. An injury was defined as any injury sustained during training or competition resulting in restricted performance or time lost from play [ 23 ]. Lower back pain (LBP) was defined as pain and discomfort localized below the costal margin and above the inferior gluteal folds, with or without leg pain [ 24 ].
2.3. Star Excursion Balance Test
The Star Excursion Balance Test comprises a single-leg balance with an oppositional reaching movement measuring the anterior, posterolateral, and posteromedial reach of both legs [ 13 ]. The test was explained and demonstrated to the participants. Before the formal testing, they practiced six trials in each direction. Participants were positioned with their foot in the center of the testing grid, which was created by aligning a series of three tape measures secured on the floor. Athletes were instructed to keep their hands on their hips, head facing forward, and to keep their stance foot flat on the floor. In that position they were instructed to reach as far as possible in the three directions with the toe of the other foot and make a single, light toe touch on the tape measure.
Reach distance was marked by the tape with the pen and then measured using a tape measure. The maximum value of three trials was used for analysis. The trial was repeated if the athlete failed to maintain a unilateral stance, lifted or moved the stance foot from the center of the grid, touched down with the reach foot, or failed to return the reach foot to the starting position. The distance reached was normalized to leg length by dividing excursion distance by leg length and they multiplying it by 100. The sum of the three reach directions divided by three times the leg length and then multiplied by 100 was used to calculate the composite scores.
2.4. Statistical Analysis
Statistical analysis was performed using SPSS 25.0 (IBM, Armonk, NY, USA). The normality of the data was checked using Shapiro–Wilk test. Descriptive statistics included the mean and standard deviation for numeric variables or frequency and percentages for categorical variables.
The Welch test was used for comparison of the SEBT scores between the group of participants without injury and the group of participants with injury in general or specific injuries and LBP. Differences in the injury rate before and after the testing were calculated using McNemar’s test.
Binary logistic regression was initially performed to examine whether normalized SEBT scores for anterior, posteromedial, and posterolateral directions of both legs; composite scores and asymmetries ≥4 cm could identify those at risk of injury in general, lower extremity injury, contact lower leg injury, non-contact lower leg injury, and lower back pain. Odds ratio (OR) and 95% confidence intervals (CI) were calculated.
Hierarchical multiple linear regression analyses were conducted to determine the impact of SEBT variables on injuries. Variables with a p value of <0.20 on the Wald test [ 25 ] in the univariate models were entered into multiple regression analyses. In these models age, previous injury, BMI, total training load, and number of training sessions per week were entered in Step 1, and SEBT variables were entered in Step 2. Tolerance and variance inflation factor (VIF) were used to check for multicollinearity. Results were considered significant at p < 0.05.
Sixty amateur soccer players were invited to participate in the study. Forty-two players accepted the invitation and fulfilled the inclusion criteria. Table 1 shows the participant’s general characteristics. Regarding their tactical position in soccer, the majority of participants (N = 19; 45.2%) had the position of midfielder. Furthermore, there were 10 (23.8%) strikers, 7 (16.7%) defenders, and 6 (14.3%) goalkeepers. Their injuries and LBP before and after the testing are presented in Table 2 . There were no significant differences in the injury and LBP rate between the period 6 months before the testing and at the end of the period 3.5 months after the testing.
General characteristics of the participants (N = 42).
N—sample; SD—standard deviation; BMI—body mass index.
Characteristics of the injuries and lower back pain among the participants (N = 42).
N—sample; LE—lower extremity; LBP—lower back pain.
The SEBT results for the total sample and according to injury status and LBP are presented in Table 3 . Significant differences were found in all directions as well as in the composite score in the SEBT results between uninjured and injured players with any injury and lower extremity injury. In addition, significant differences were found in the anterior direction of both the dominant and non-dominant leg between those with and without LBP. None of the participants had anterior asymmetry ≥4 cm; however, 5 (11.9%) participants had posteromedial asymmetry ≥4 cm. Four (9.5%) participants had posterolateral asymmetry ≥4 cm. All but one participant had their SEBT score <89.6%.
SEBT results for the total sample and according to injury status and LBP.
N—sample; SD—standard deviation; LE—lower extremity; LBP—low back pain; ANT—anterior; PMED—posteromedial; PLAT—posterolateral; LL—normalized score; * statistically significant.
Table 4 shows the SEBT results according to lower extremity injury mechanism. There were no significant differences between those with and without a contact and non-contact mechanism of injury.
SEBT results according to LE injury mechanism.
N—sample; SD—standard deviation; LE—lower extremity; ANT—anterior; PMED—posteromedial; PLAT—posterolateral; LL—normalized score.
Table 5 presents results of univariate logistic regression analysis for injuries and LBP as well as ORs with their 95% CI. Shorter distance in all directions of SEBT as well as a lower composite score for both the dominant and non-dominant lower extremities were associated with any injury. Shorter distance in all but the anterior direction of the dominant leg as well as lower composite scores were associated with lower extremity injury. Only the anterior reach of the non-dominant leg was associated with LBP.
Univariate logistic regression analysis for injuries and LBP.
LE—lower extremity; LBP—low back pain; ANT—anterior; PMED—posteromedial; PLAT—posterolateral; LL—normalized score; * statistically significant.
The results of the univariate logistic regression analysis for contact and non-contact lower extremity injuries are shown in Table 6 . No directions of the SEBT nor the composite score could correctly identify those at risk of contact or non-contact lower extremity injury. Posteromedial and posterolateral asymmetries ≥4 cm could not identify those at risk of injury or LPB.
Univariate logistic regression analysis for contact and non-contact LE injuries.
LE—lower extremity; ANT—anterior; PMED—posteromedial; PLAT—posterolateral; LL—normalized score.
Multiple regression analysis revealed that age, previous injury, BMI, total training load, and number of training sessions per week explained 28% of the injury variance, while the composite score for the non-dominant leg added an extra 13% ( Table 7 ). There was a positive association between BMI and injury, and negative associations between training load, SEBT composite score of the non-dominant leg, and injury in general. Age, previous, injury, BMI, total training load, and number of training sessions per week explained 47% of the lower extremity injury variance. The composite score for the non-dominant leg added an extra of 11%. There were negative associations between training load and the SEBT composite score of the non-dominant leg and lower extremity injury. Other SEBT variables did not contribute to neither model.
Multiple regression analysis examining the contribution of age, previous injury, BMI, training load, and selected SEBT variables to injury and LE injury.
* p < 0.05, ** p < 0.01; SE—standard error; b—unstandardized coefficient; β—standardized coefficient.
4. Discussion
This study aimed to examine if there is a relationship between SEBT reach distances and musculoskeletal injury and LBP among non-professional soccer players. Furthermore, it aimed to determine whether the SEBT scores can be used in the prediction of injuries and LBP. The results partially confirmed our hypothesis. Shorter reach distances in all directions and lower composite score were associated with musculoskeletal injury in general. Likewise, shorter reach distances in all but the anterior direction of the dominant leg and a lower composite score were associated with lower extremity injury. LBP was associated with a shorter reach distance in the anterior direction of the non-dominant leg. However, SEBT results could not identify those at risk of specific lower extremity injuries. Asymmetries in posterolateral and posteromedial directions ≥4 cm could not identify those at risk of injury or LBP. To the best of our knowledge, only one previous study investigated predictive value of the SEBT in non-professional soccer players. This adds some new aspects regarding the association between the SEBT and musculoskeletal injury and LBP in very specific population, amateur soccer players, with the possibility to lower the risk of injuries and LBP by using screening and implementing prevention strategies according to the results of the screening. We specifically selected this population because there were not enough previous studies which included amateur athletes and data in the literature for professional athletes cannot be generalized to amateur athletes.
A previous similar study performed by Gonell et al. [ 26 ], which examined the relationship between modified SEBT scores and soft tissue injury incidence in a soccer team, included a total of 74 soccer players. Forty of these participants were amateur athletes. All reach directions, including the composite score, exceeded values of the results in our sample; however, the results were similar to ours, showing an increased risk of injury with decreased reach directions of the SEBT. A significant relationship was found between below the average normalized anterior reach distance and contact injuries, as well as below the average normalized posteromedial reach distance and non-contact injuries. Below the average values of the normalized posterolateral reach distance and normalized composite reach distance were related to an increased risk of total and non-contact injuries. Participants with a composite reach distance below the average of the sample were approximately two times more likely to sustain an injury.
Another previous study examining the predictive value of SEBT scores on lower extremity injuries was performed by Plisky et al. [ 13 ]. They investigated whether SEBT reach distance was associated with the risk of lower extremity injury among high school basketball players, which makes their sample quite different than ours. However, their results were similar. They reported that an anterior right/left reach distance difference ≥4 cm, decreased the normalized right anterior reach distance and decreased the normalized posteromedial, posterolateral, and composite reach distances bilaterally were significantly associated with lower extremity injury.
O’Connor et al. [ 27 ] examined whether modified SEBT results can identify those at risk of contact or non-contact lower extremity injury in a population of adolescent and collegiate footballers and hurlers. Poor scores were unable to ascertain those at risk of contact or non-contact lower extremity combined and ankle injuries with sufficient sensitivity. Contrary to that, a study performed by Ko et al. [ 28 ] established that the posteromedial and posterolateral reach of the SEBT can identify adolescent athletes who will incur a subsequent lateral ankle sprain. Indeed, the literature reported that asymmetry in the anterior direction is more common among those with a history of lateral ankle sprain in comparison to those without [ 29 ]. In our study, we did not find asymmetries related to future injuries; however, ankle sprain was not specifically taken into account.
Research by Ganesh et al. [ 18 ] reported on significant reductions in excursion distances for all directions of the SEBT in group of subjects with lower back pain. Contrary to that, another study investigating SEBT results in young athletes with back pain did not find significant differences between the reach distances in all three directions of those with and without back pain [ 30 ]. In our study, we find only differences in the anterior reach for both the dominant and non-dominant leg between those with and without LBP. In addition, a shorter distance of the anterior reach of the non-dominant leg was associated with the occurrence of LBP.
Indeed, impaired balance is established as a risk factor for lower limb injury [ 31 ]. Neuromuscular risk factors for lower extremity injury in male soccer players include m. quadriceps dominance, leg dominance (asymmetry), knee valgus, trunk dominance, and reduced dynamic stability [ 32 ]. Furthermore, previous research reported impaired postural control in LBP and proposed that balance impairment in LBP patients correlates with deficits in the musculoskeletal and neural systems [ 33 , 34 ]. Controlling balance requires the interaction of the neurological, musculoskeletal, proprioceptive, vestibular, and visual systems [ 18 ]. Therefore, it is very important to develop and validate appropriate screening methods for assessments of neuromuscular control, including balance, with the goal of identifying those which may be at a greater risk of injury or LBP.
We have demonstrated that the SEBT can be a useful and simple method of clinical screening in amateur soccer players. The test could be incorporated into the pre-participation screening of athletes to help identify those at risk of injury or LBP. These deficits could be improved through a neuromuscular training program prior to the competitive season. There is the need to establish cut-off points, which will be population- and sport-specific, in order to more accurately determine the future injury risk. Cut-off points and previous research on professional soccer players are not generalizable to the amateur athlete population due to different training loads and the frequency of training sessions and competitions.
Our study’s prospective design allowed us to minimize recall bias regarding the injuries. However, our study had some limitations. First, our sample was small and consisted of only male amateur soccer players from three soccer clubs. This makes difficult to generalize our results to other populations of athletes. Furthermore, the follow-up period was relatively short. Future studies should consider a larger sample consisting of both genders from different sports, and a longer period of follow up. It is also important to note that we examined only the results of the SEBT in terms of injury prediction, and we did not take into account many of the other variables that could influence the risk of injury and LBP. Strong points of the study include the use of a valid and reliable test, a homogenous population, and the prospective design.
5. Conclusions
In conclusion, our data suggests the predictive value of the SEBT for injuries in general, lower extremity injuries, and LBP occurrence. It seems that amateur soccer players with lower SEBT scores are more prone to injuries in general, as well as injuries of the lower extremities. Amateur soccer players have different training loads and lifestyle in comparison to professional athletes, and there is also lack of financial resources for the amateur soccer clubs. However, use of simple screening procedures could have a positive impact on injuries and LBP. Further studies are needed to confirm these findings and to establish specific cut-off points, which would allow more precise predictions.
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization, I.S.K., K.P. and T.K.; methodology, I.S.K. and D.K.; software, K.P.; validation, I.S.K. and S.J.; formal analysis, I.S.K., S.J. and D.K.; investigation, K.P. and S.J.; data curation, I.S.K.; writing—original draft preparation, K.P., S.J. and T.K.; writing—review and editing, I.S.K. and D.K.; supervision, I.S.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and was approved by the Ethics Committee for Biomedical Research, Faculty of Health Studies, University of Rijeka, Croatia (21 February 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
Star excursion balance test scores under different conditions: Effects of arms position and shoe-wear
Affiliations.
- 1 Hacettepe University, Faculty of Physical Therapy and Rehabilitation, Ankara, Turkey. Electronic address: [email protected].
- 2 Hacettepe University, Faculty of Physical Therapy and Rehabilitation, Ankara, Turkey.
- PMID: 35500967
- DOI: 10.1016/j.jbmt.2021.10.011
Objectives: The purpose of this study was to investigate the effects of arms position (arms free or hands on the hips) and shoe-wear (with or without athletic shoe) on star excursion balance test (SEBT) scores in healthy physically active individuals.
Design: Cross-sectional study.
Methods: Fifty-one participants [Age: 22.74 ± 1.93 years; Body Mass Index: 22.52 ± 2.29 kg/m 2 ] were included in the study. The anterior (ANT), posteromedial (PM) and posterolateral (PL) reach directions of the SEBT were performed under four conditions in a randomized order. Within session reliability analysis was performed for each test condition. The composite (COMP) score was calculated as the average of the normalized scores of anterior, posteromedial and posterolateral reach distances. Repeated measures of ANOVA was used for statistical analysis.
Results: The ANT and PM reach distances and the composite (COMP) score were found greater with shoes (ANT p = 0.004; PM p < 0.001; COMP p < 0.001). However, the difference in the scores with shoes conditions did not exceed the measurement error. On the other hand, PM and PL reach distances and the COMP score were greater with arms free conditions and the difference in the scores exceeded the measurement error.
Conclusions: The results of the study suggest that the differences in the SEBT procedure should be taken into account when comparing the outcomes of different studies. In addition, measurement error values should be considered while interpreting the change in repeated measures of SEBT scores.
Keywords: Dynamic balance; Functional performance; Postural control; Reliability.
Copyright © 2021 Elsevier Ltd. All rights reserved.
- Cross-Sectional Studies
- Postural Balance
- Reproducibility of Results
- Young Adult

IMAGES
VIDEO
COMMENTS
The Star Excursion Balance Test (SEBT) is a dynamic test that requires strength, flexibility, and proprioception. It is a measure of dynamic balance that provides a significant challenge to athletes and physically active individuals. ... = Average distance in each direction / leg length * 100; These calculations should be performed for both the ...
The Star Excursion Balance Test (SEBT) is a test of dynamic balance, using in a single-leg stance that requires strength, flexibility, core control and proprioception. The test requires participants to balance on one leg and reach as far as possible in eight different directions. ... Calculate Average distance in each direction (average of the ...
The Star Excursion Balance Test (SEBT) is a reliable, responsive, and clinically relevant functional assessment of lower limbs' dynamic postural control. However, great disparity exists regarding its methodology and the reported outcomes. Large and specific databases from various population (sport, age, and gender) are needed to help clinicians when interpreting SEBT performances in daily ...
The Star Excursion Balance Test (SEBT) is a relatively simple, but somewhat time-intensive, test used to measure dynamic balance, otherwise known as dynamic postural control (1). It measures dynamic balance by challenging athletes to balance on one leg and reach as far as possible in eight different directions (2). ... Average distance in each ...
The authors considered that because men on average are taller and have longer limbs than women, perhaps a normalizing procedure should be implemented. ... The search terms included Star Excursion Balance Test and SEBT. Study Selection. The criteria for article selection were (1) The study was original research. (2) The study was written in ...
At the end of the Star Excursion Balance Test, the patient should have completed 3 full circuits with both legs and the distance of each trial should be measured. Scoring: To score the SEBT, first calculate the average reach distance in each direction in centimeters, by dividing the sum of all 3 trials per leg through 3. So you should have 16 ...
The Star Excursion Balance Test (SEBT) is a reliable, responsive, and clinically relevant functional assessment of lower limbs' dynamic postural control. However, great disparity exists regarding ...
The Star Excursion Balance Test (SEBT) is a reliable, responsive, and clinically relevant functional assessment of lower limbs' dynamic postural control. ... redundancy of testing directions while maintaining consistency and reliability from the original SEBT.16,26 The average of the three directions is then often calculated to create a ...
N The Star Excursion Balance Test should be considered a highly representative noninstrumented dynamic balance test for physically active people. N The Star Excursion Balance Test is a reliable measure and a valid dynamic test to predict risk of lower extremity injury, to identify dynamic balance deficits in patients with lower extremity ...
A comparison of Star Excursion Balance Test reach distances between ACL defiient patients and asymptomatic controls. The Knee 16 (2009) 149-152. Hertel J, Braham RA, Hale SA, Olmsted Kramer LC. Simplifying the Star Excursion Balance Test: Analyses of Subjects With and Without Chronic Ankle Instability. J Orthop Sports Phys Ther 2006;36:131-137.
In particular, the Star Excursion Balance Test (SEBT) has become a popular clinical assessment of dynamic balance and postural control. As the SEBT requires a combination of lower extremity strength, coordination, balance, and flexibility,6,12,22,26 the test has the capability to identify athletes at risk. TSTUDY T DESIGN: Cross-sectional.
balance and proprioception May 22, 2023. 1:12. The Star Excursion Balance Test (SEBT) is one of our favourite tests and one of the major reasons we developed the MAT to rid the world of ugly pieces of sports tape stuck to the floor of clinics and gyms everywhere. This assessment has been well researched to demonstrate high inter and intra ...
The Star Excursion Balance Test (SEBT) is one of my favourite dynamic balance assessment tools and this blog covers the construct and current literature existing around it's use. The SEBT is not an injury-specific test and has been the subject of research for almost 20 years, and was first described in 1998 (Gribble, Hertel & Plisky., 2012).
The Star Excursion Balance Test (SEBT) is a valid and reliable outcome measure of dynamic balance developed by Gray. 3 A range of indications for the clinical use of the test in athletic and pathologic populations has previously been described, including screening, 4, 5 injury identification, 6, 7 training, 8 - 10 and rehabilitation. 11 Most ...
The 'Y-test' is a test that is comparable to the SEBT but uses only three directions. Scoring System of Star Excursion Balance Test. All distances reached during the test are recorded to the closest 0.5 cm. Calculate the average of the three measurements for each direction, as well as the relative distance in each direction (normalized) (%) (average distance in each direction/leg length ...
Abstract and Figures. Background: Star Excursion Balance Test (SEBT) is a simple, reliable, cost effective screening test which is used to evaluate the dynamic balance of lower limbs in 8 ...
The Star Excursion Balance Test (SEBT) is a common assessment used across clinical and research settings to test dynamic standing balance. ... Blazepod™ (BlazePod Inc., Miami, FL, USA) sensors were then placed on the average maximum reaching distances for each participant. Blazepod TM sensors are reactive lights seen in Figure 1, which turn ...
Star Excursion Balance Test The Star Excursion Balance Test is a rehabilitation tool that uses a series of single-limb squats and reaching tasks to assess dynamic postural control (how well you can keep your ... Perform 3 trials for each line/direction and record the average score. Swap legs and repeat the test.
Despite the recognized importance of neuromuscular exercises, there is currently no widely accepted clinical outcome measure focused on neuromuscular control for patients with knee osteoarthritis (OA). The purposes of the present study were to investigate the test-retest reliability, concurrent validity and longitudinal validity of the star excursion balance test (SEBT) in patients with knee OA.
The Star Excursion Balance Test (SEBT) as a practical test for ankle function and the Foot and Ankle Disability Index (FADI) as a questionnaire in order to assess quality of life, depending on the ...
The Star Excursion Balance Test comprises a single-leg balance with an oppositional reaching movement measuring the anterior, posterolateral, and posteromedial reach of ... Below the average values of the normalized posterolateral reach distance and normalized composite reach distance were related to an increased risk of total and non-contact ...
Star excursion balance test scores under different conditions: Effects of arms position and shoe-wear J Bodyw Mov Ther. 2022 Apr; 30:17-22. ... (COMP) score was calculated as the average of the normalized scores of anterior, posteromedial and posterolateral reach distances. Repeated measures of ANOVA was used for statistical analysis.